109669
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

已发表论文
纤维化畸形血管: 独特的血管发育异常,可导致痔疮疾病
Authors Li SL, Jing FY, Ma LL, Guo LL, Na F, An SL, Ye Y, Yang JM, Bao M, Kang D, Sun XL, Deng YJ
Received 9 June 2015
Accepted for publication 2 July 2015
Published 13 August 2015 Volume 2015:9 Pages 4649—4656
DOI http://dx.doi.org/10.2147/DDDT.S90209
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Rekha Dhanwani
Peer reviewer comments 2
Editor who approved publication: Professor Wei Duan
Background: The etiology and pathogenesis of hemorrhoids is unclear, although hemorrhoids are a worldwide disease in men and women, with peak prevalence at 45–65 years of age. Hemorrhoidal cushions as the anal venous plexi are normal anatomical structures from infancy. This study attempts to reveal the angiodysplasia and other pathological changes in association with different degrees of symptomatic hemorrhoids.
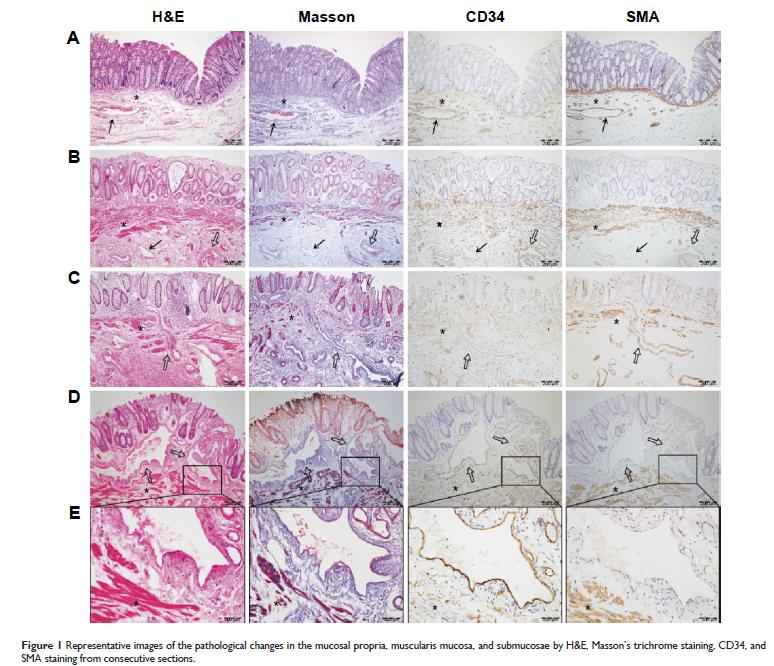
Materials and methods: A total of 281 patients with internal hemorrhoids from degree I to IV underwent hemorrhoidectomy. The vascular changes were analyzed by microscopic assessment and software analysis, with Masson’s trichrome, CD34, and smooth muscle actin.
Results: The hemorrhoidal tissues exhibited abnormal vessels in the mucosae and submucosae that we termed them as myofibrotic malformation vessels (MMVs). MMVs are not ascribed to arteries or veins because they exhibit enlarged and tortuous lumens with smooth
muscle dysplasia and fibrotic deposition in the walls without overlying mucosal ulceration. The muscularis mucosae also showed smooth muscle dysplasia and fibrosis, even if it were interrupted by the intruding MMVs. The statistical data indicated that the severity of all the changes correlate positively with the progression of hemorrhoids (P <0.001). Hemorrhoidal patients are prone for reoccurrence even with prolapsing hemorrhoid when compared with the conventional hemorrhoidectomy. Multiple logistic regression analysis showed that MMVs in mucosal propria, mean thickness of mucosal muscularis layer, and fibrotic changes in MMV were independent risk factors for MMVs in hemorrhoidal disease.
Conclusion: MMVs and muscularis mucosae dysplasia reciprocally contribute to hemorrhoidal exacerbation. The novel findings of this study propose that the characteristic features of MMVs and muscularis mucosae dysplasia of the anorectal tube ultimately cause symptomatic hemorrhoids, which could affect the clinical management of hemorrhoidal disease through the use of surgery to target the malformed vessels.
Keywords:internal hemorrhoids, hemorrhoidal progression, myofibrotic malformation vessels, muscularis mucosae dysplasia, anorectal disease
Materials and methods: A total of 281 patients with internal hemorrhoids from degree I to IV underwent hemorrhoidectomy. The vascular changes were analyzed by microscopic assessment and software analysis, with Masson’s trichrome, CD34, and smooth muscle actin.
Results: The hemorrhoidal tissues exhibited abnormal vessels in the mucosae and submucosae that we termed them as myofibrotic malformation vessels (MMVs). MMVs are not ascribed to arteries or veins because they exhibit enlarged and tortuous lumens with smooth
muscle dysplasia and fibrotic deposition in the walls without overlying mucosal ulceration. The muscularis mucosae also showed smooth muscle dysplasia and fibrosis, even if it were interrupted by the intruding MMVs. The statistical data indicated that the severity of all the changes correlate positively with the progression of hemorrhoids (P <0.001). Hemorrhoidal patients are prone for reoccurrence even with prolapsing hemorrhoid when compared with the conventional hemorrhoidectomy. Multiple logistic regression analysis showed that MMVs in mucosal propria, mean thickness of mucosal muscularis layer, and fibrotic changes in MMV were independent risk factors for MMVs in hemorrhoidal disease.
Conclusion: MMVs and muscularis mucosae dysplasia reciprocally contribute to hemorrhoidal exacerbation. The novel findings of this study propose that the characteristic features of MMVs and muscularis mucosae dysplasia of the anorectal tube ultimately cause symptomatic hemorrhoids, which could affect the clinical management of hemorrhoidal disease through the use of surgery to target the malformed vessels.
Keywords:internal hemorrhoids, hemorrhoidal progression, myofibrotic malformation vessels, muscularis mucosae dysplasia, anorectal disease