108985
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

临床上重要的气单胞菌属独特的抗菌素耐药性图谱在中国西南地区:一项为期七年的监测研究
Authors Yang S, He T, Sun J, Sun S
Received 24 May 2019
Accepted for publication 4 September 2019
Published 18 September 2019 Volume 2019:12 Pages 2971—2978
DOI https://doi.org/10.2147/IDR.S216926
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Dr Joachim Wink
Background: Co-evolution of host and aeromonads has diversified their spectrums of diseases and antibiograms, while a paucity of data was concerning about this diversity in China. To fill this gap, this study was aimed to investigate and compare antimicrobial resistance (AMR) patterns of clinically important Aeromonas spp. from various clinical sources.
Methods: A multicenter retrospective surveillance study was conducted in Chongqing from 2011 to 2017. Data of strains were retrieved from the database of China Antimicrobial Resistance Surveillance System (CARSS). Whonet 5.6 and Graphpad Prism 6 Software were adopted to determine and compare distribution and AMR patterns.
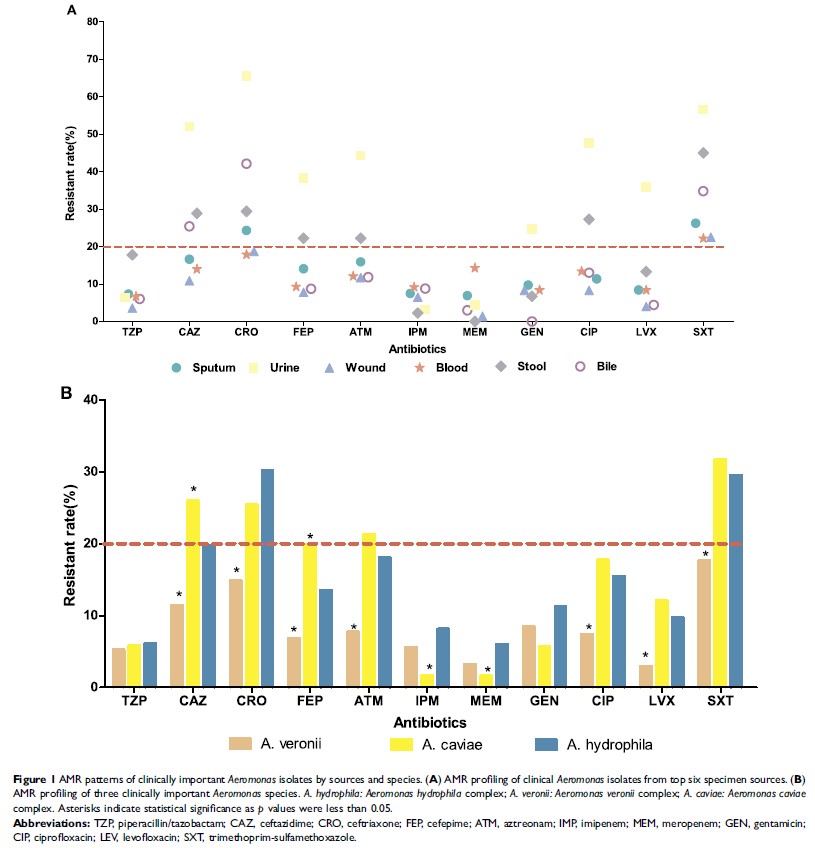
Results: Among 1135 Aeromonas strains, Aeromonas hydrophila complex (65.6%, 745/1135) was the most predominant species, followed by Aeromonas veronii complex (16.7%, 190/1135) and Aeromonas caviae complex (15.3%, 174/1135). Sputum was the most frequent source of strains (27.7%), followed by wound (20.8%), bloodstream (10.8%) and urine (8.8%). Urinary strains demonstrated the highest resistance rates to ceftriaxone (65.6%), ceftazidime (52.1%), cefepime (38.3%), ciprofloxacin (47.7%) and trimethoprim-sulfamethoxazole (56.6%). Similar AMR pattern was observed in intestinal strains, with corresponding resistance rates of 29.4%, 28.9%, 22.2%, 27.3% and 45%, respectively. However, respiratory, bloodstream and skin strains exhibited resistance rates of less than 20% to most of the antimicrobials tested. In terms of species, approximately 30% of Aeromonas hydrophila complex and Aeromonas caviae complex strains were resistant to ceftriaxone and trimethoprim-sulfamethoxazole, while Aeromonas veronii complex strains harbored resistance rates of less than 20% to all tested antimicrobials. Although antibiograms of these species were distinct, they remained constant from 2011 to 2017.
Conclusions: Distinct AMR patterns between species and sources highlighted the predominance of Aeromonas hydrophila complex and high resistance of strains in urine and intestine to extended-spectrum cephalosporins, ciprofloxacin and trimethoprim-sulfamethoxazole in Southwest China. Temporally constant AMR patterns should not relax the vigilance of antimicrobial resistance in clinically important Aeromonas species.
Keywords: Aeromonas , human, antimicrobial resistance, distribution, time trend