108985
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

在大肠肝有限转移的转换治疗中肝脂肪变性的预测价值和预后价值:倾向评分匹配分析
Authors Jian M, Chang W, Ren L, Liu T, Chen Y, Wei Y, Lin Q, Xu J, Qin X
Received 28 March 2019
Accepted for publication 1 September 2019
Published 11 September 2019 Volume 2019:11 Pages 8315—8326
DOI https://doi.org/10.2147/CMAR.S210185
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Cristina Weinberg
Peer reviewer comments 3
Editor who approved publication: Professor Bilikere Dwarakanath
Purpose: To evaluate the role of hepatic steatosis (HS) in patients with synchronous colorectal liver-limited metastases (CLLMs) undergoing conversion therapy.
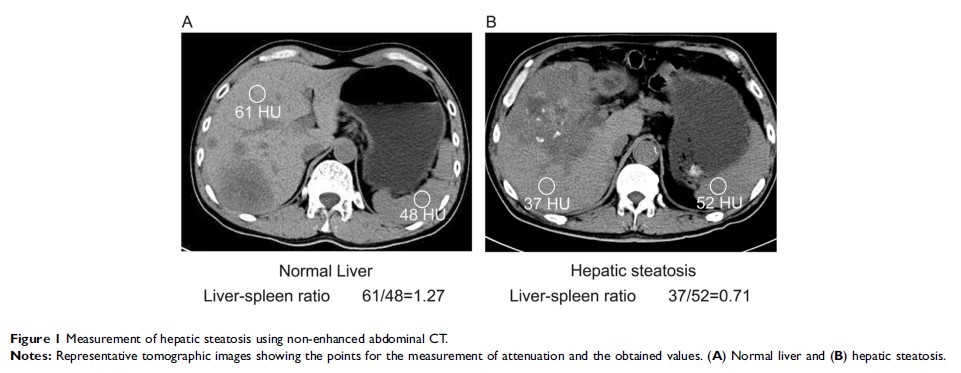
Patients and methods: From March 2013 to March 2017, a total of 406 patients with initially unresectable CLLMs accepted conversion therapy in multidisciplinary team (MDT). Before the implementation of conversion therapy, all patients underwent CT scan to assess the presence of hepatic steatosis and divided into the HS group (n = 124) and the non-HS group (n = 282). After using propensity score matching (PSM) to eliminate the potential confounding bias of the two groups, the conversion hepatectomy rate and long-term oncological survival in two groups were compared.
Results: After 1:1 PSM, no significant difference was observed at baseline between patients in the HS group (n = 119) and the non-HS group (n = 119). Patients in the HS group had higher conversion hepatectomy rate from MDT evaluation (31.1% vs 18.5%, P = 0.029) and actual hepatectomy rate (30.2% vs 18.5%, P = 0.030), when compared with patients in the non-HS group, respectively. In addition, the HS group achieved better progression-free survival (PFS, P = 0.047) and overall survival (OS, P = 0.035) than that of the non-HS group. Multivariate logistic analysis confirmed that pretreatment HS was an independent predictor for conversion hepatectomy rate (OR, 2.393; 95% CI, 1.463–4.315, P = 0.001), and multivariate Cox analysis revealed that HS was an independent prognostic factor for PFS (HR, 0.493, 95% CI 0.281–0.866, P = 0.014) and OS (HR, 0.559, 95% CI 0.398–0.785, P = 0.001).
Conclusion: For CLLM patients who underwent conversion therapy, hepatic steatosis could be an effective predictor for conversion hepatectomy rate and an independent prognostic factor for PFS and OS.
Keywords: colorectal cancer, liver metastases, conversion therapy, hepatic steatosis, objective response rate, survival