108985
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

腹腔镜根治性子宫切除术的不良反应取决于宫颈癌患者的肿瘤大小
Authors Hu TWY, Ming X, Yan HZ, Li ZY
Received 24 May 2019
Accepted for publication 5 August 2019
Published 9 September 2019 Volume 2019:11 Pages 8249—8255
DOI https://doi.org/10.2147/CMAR.S216929
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Nicola Ludin
Peer reviewer comments 2
Editor who approved publication: Dr Antonella D'Anneo
Purpose: The study aimed to explore the survival outcomes of early-stage cervical cancer (CC) patients treated with laparoscopic/abdominal radical hysterectomy (LRH/ARH).
Patients and Methods: We performed a retrospective analysis involving women who had undergone LRH/ARH for CC in early stage during the 2013–2015 period in West China Second University Hospital. The survival outcomes and potential prognostic factors were evaluated using Kaplan–Meier method and Cox regression analysis, respectively.
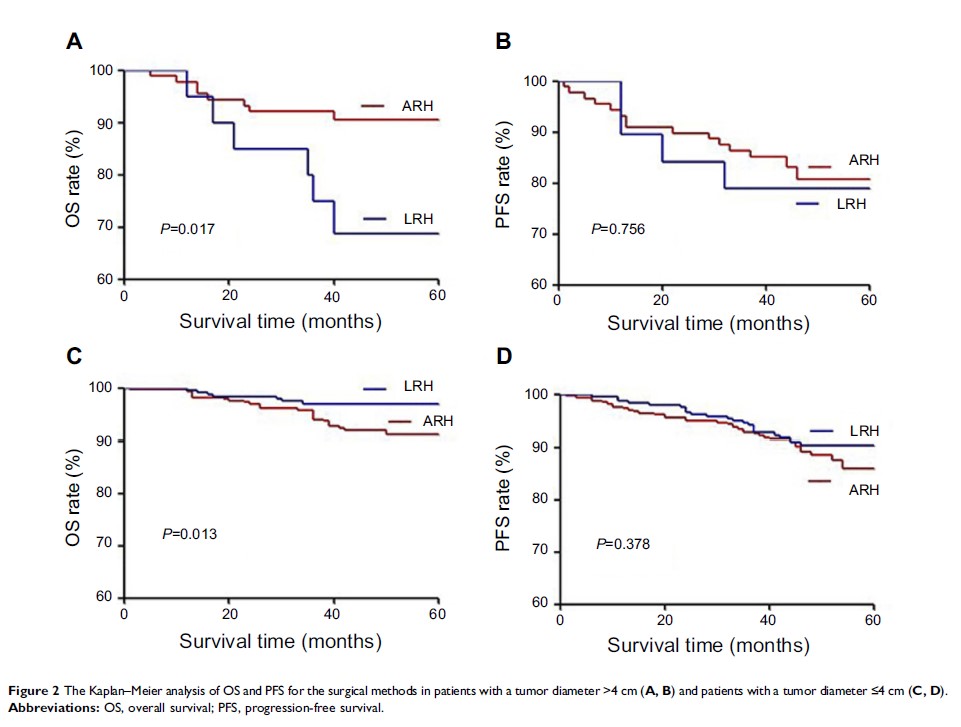
Results: A total of 678 patients were included in our analysis. The overall survival (OS) and progression-free survival (PFS) between the ARH (n=423) and LRH (n=255) groups achieved no significant differences (p =0.122, 0.285, respectively). However, in patients with a tumor diameter >4 cm, the OS of the LRH group was significantly shorter than that of the ARH group (p =0.017). Conversely, in patients with a tumor diameter ≤4 cm, the LRH group had a significantly longer OS than the ARH group (p =0.013). The multivariate Cox analysis revealed that International Federation of Gynecology and Obstetrics stage, histology, parametrial invasion, and pelvic lymph node invasion were independent prognostic factors for OS and PFS, whereas surgical method was not a statistically significant predictor of OS (p =0.806) or PFS (p =0.236) in CC patients.
Conclusion: LRH was an alternative to ARH for surgical treatment of CC patients with a tumor diameter ≤4 cm. However, for the patients with a tumor diameter >4 cm, priority should be given to ARH.
Keywords: cervical cancer, laparoscopy, hysterectomy, prognosis