108985
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

系统性炎症及短期抗生素治疗对稳定期 COPD 的 PPM 阳性患者的影响
Authors Wang JX, Li HQ, Zhang F, Ning W
Received 1 June 2019
Accepted for publication 12 August 2019
Published 23 August 2019 Volume 2019:14 Pages 1923—1932
DOI https://doi.org/10.2147/COPD.S217971
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Nicola Ludin
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Chunxue Bai
Objective: To evaluate patients with stable COPD for the presence of potentially pathogenic microorganisms (PPM), systemic inflammation and the effects of short-term antibiotic therapy in PPM positive patients.
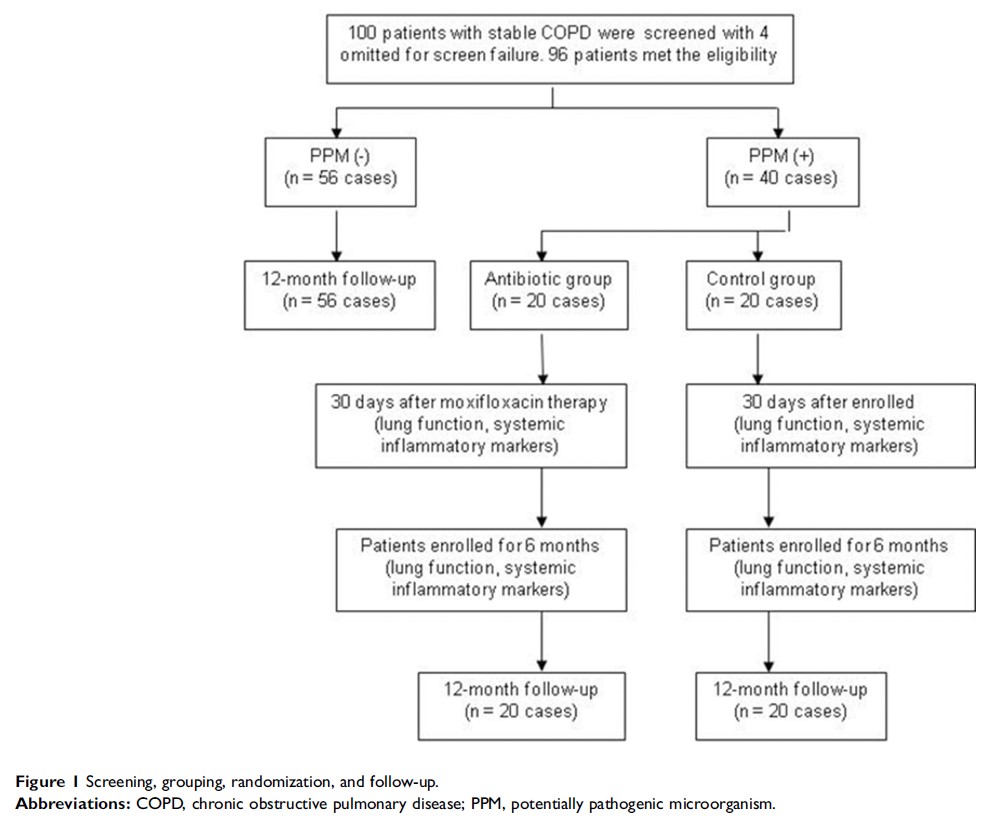
Methods: From January 2016 to June 2017, we enrolled 96 stable COPD patients. Bacterial cultures from sputum collections were quantitated, along with markers for systemic inflammation including serum C-reactive protein (CRP), interleukin-8 (IL-8) and plasma fibrinogen (FIB) in all patients. All enrolled patients were followed for 12 months. Forty patients were identified as PPM positive and were randomly divided into an antibiotic group and a control group. The antibiotic group was treated with moxifloxacin orally for 6 days. Lung function and markers for systemic inflammation were repeatedly measured at 30 days and 6 months in PPM positive subjects.
Results: Binary logistic regression analysis showed that risk factors for PPM positive are bronchiectasis (OR 4.18, 95% CI 1.20–14.59; P =0.025), COPD assessment test (CAT) ≥20 (OR 17.55, 95% CI 2.82–109.18; P =0.002), spontaneous sputum (OR 15.09, 95% CI 1.36–168.02; P =0.027) and sputum purulence (OR 38.43, 95% CI 5.39–274.21; P =0.000). CRP and IL-8 were higher in PPM positive group than those in PPM negative group (P =0.001, P =0.007, respectively), but there were no differences of FIB between the two groups (P =0.086). Compared to the PPM negative group, the rate of acute exacerbation of COPD was higher (P =0.029) and time to next acute exacerbation was shorter (P =0.030) in PPM positive group. There were no differences in lung function and systemic inflammatory markers either in the control group or the antibiotic group at different time points of follow-up.
Conclusion: PPM exists in stable COPD patients and can cause systemic inflammation and is associated with acute exacerbation of COPD. Short-term antibiotic therapy had no effect on systemic inflammation nor on acute exacerbation of COPD.
China Clinical Trials Registry: ChiCTR-IOR-15006769
Keywords: COPD, potentially pathogenic microorganisms, systemic inflammation, antibiotics, C-reactive protein, interleukin-8