108985
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

中国三级医疗结核病医院耐药结核病的患病率、风险和遗传特征
Authors Zhao LL, Huang MX, Xiao TY, Liu HC, Li MC, Zhao XQ, Liu ZG, Jiang Y, Wan KL
Received 25 March 2019
Accepted for publication 4 July 2019
Published 7 August 2019 Volume 2019:12 Pages 2457—2465
DOI https://doi.org/10.2147/IDR.S209971
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Cristina Weinberg
Peer reviewer comments 2
Editor who approved publication: Dr Joachim Wink
Objectives: To explore the prevalence, risk and genetic characteristics of drug-resistant tuberculosis (TB) from a tertiary care TB hospital in China.
Patients and methods: We carried out a retrospective study including isolates from 189 patients with pulmonary TB at Fuzhou Pulmonary Hospital. All isolates from these patients were subjected to drug susceptibility testing and genotyping. For drug-resistant isolates, DNA sequencing was used to investigate mutations in 12 loci, including katG , inhA , oxyR–ahpC , rpoB , rpsL , rrs 1 (nucleotides 388–1084 of rrs), embB , tlyA , eis , rrs 2 (nucleotides 1158–1674 of rrs), gyrA and gyrB .
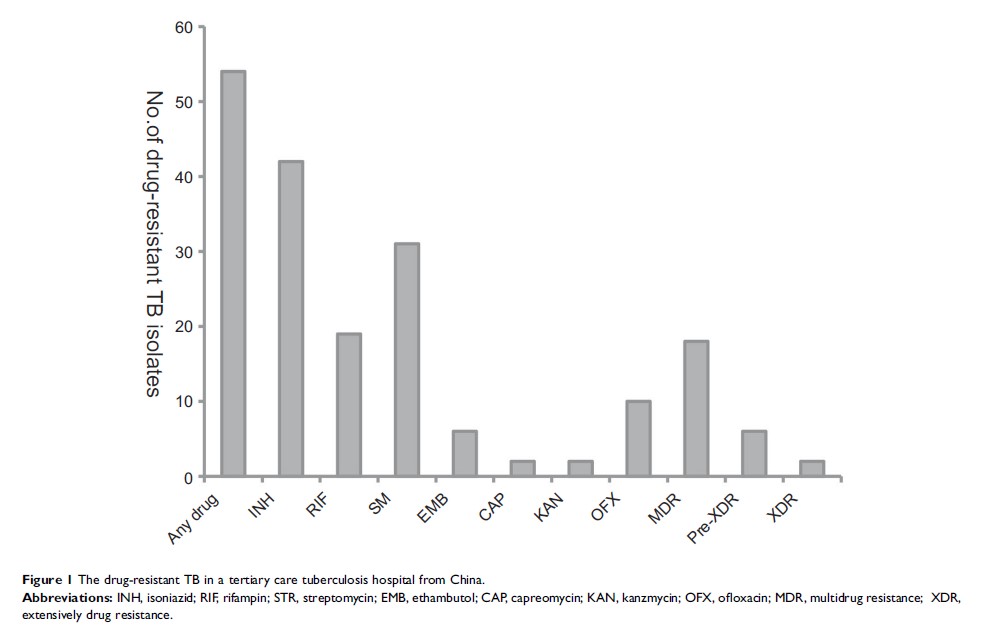
Results: Among 189 isolates, 28.6% were resistant to at least one of the seven anti-TB drugs, including isoniazid (INH), rifampin (RIF), streptomycin (STR), ethambutol (EMB), capreomycin (CAP), kanzmycin (KAN) and ofloxacin (OFX). The proportion of multidrug-resistant TB and extensively drug-resistant TB isolates was 9.5% and 1.1%, respectively. Patients in rural areas as well as previously treated patients showed a significantly increased risk of developing drug resistance. In addition, among these isolates, 111 (58.7%) were Beijing genotype strains, 84 (75.7%) of which belonged to modern Beijing sublineage. There was no association between genotype and drug resistance. The most common mutations were katG 315, rpoB 531 rpsL 43, embB 306, rrs 1401 and gyrA 94.
Conclusion: These findings provided additional information of drug-resistant TB in China. Previously treated patients and patients in rural areas should receive greater attention owing to their higher risk of developing drug resistance.
Keywords: drug-resistant tuberculosis, genotype, risk, mutation