108985
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

胸腔镜手术后锯齿前路阻滞对局部麻醉浸润术后镇痛的影响:一项随机临床试验
Authors Chen G, Li Y, Zhang Y, Fang X
Received 28 February 2019
Accepted for publication 2 July 2019
Published 1 August 2019 Volume 2019:12 Pages 2411—2417
DOI https://doi.org/10.2147/JPR.S207116
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Melinda Thomas
Peer reviewer comments 2
Editor who approved publication: Dr Michael Ueberall
Background: Serratus anterior plane (SAP) block is a relatively novel technique that can block the lateral cutaneous branches of the intercostal nerves as well as the long thoracic nerve.
Purpose: Our study aimed to evaluate the effects of SAP block on postoperative pain after thoracoscopic surgery compared with local anesthetic (LA) infiltration.
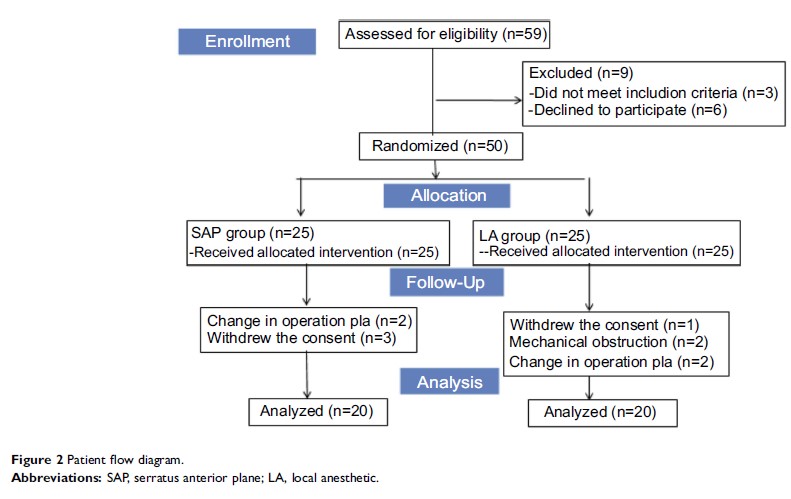
Patients and methods: Forty adult patients undergoing video-assisted thoracic surgery were randomized to receive either SAP block (n=20) or LA infiltration of incision (n=20). The primary outcome was postoperative visual analog scale (VAS) score at the 2nd, 8th, 16th, 24th, and 48th hour after surgery. The secondary outcomes were the consumption of sufentanil at 8th, 16th, 24th hours postoperative. In addition, rescue analgesia, drug-related adverse effects after surgery was also analyzed.
Results: The SAP group showed lower VAS scores at the 2nd hour (at rest: SAP group 11 [8–13] vs LA group 28 [26–32], P =0.01; on coughing: 15 [13–18] vs 33 [26–38], P =0.01) and the 8th hour (at rest: 13 [12–18] vs 36 [32–46], P =0.01; on coughing: 19 [16–23] vs 42 [36–53], P =0.01) after surgery. Postoperative sufentanil consumption in the SAP group during 0–8 hrs was significantly lower compared with the LA group (P <0.01). The use of rescue analgesia was also significantly lower in the SAP group (P =0.02) during 0–12 hrs.
Conclusion: Compared to LA infiltration, ultrasound-guided SAP block may provide better pain relief as well as reduce opioid consumption after thoracoscopic surgery.
Keywords: serratus anterior plane block, thoracoscopic surgery, local anesthetic infiltration