108985
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

在使用孕激素启动的卵巢刺激方案进行试管受精(IVF)时应用地屈孕酮对出生婴儿的新生儿影响和先天性畸形:一项回顾性队列研究
Authors Huang J, Xie Q, Lin J, Lu X, Wang N, Gao H, Cai R, Kuang Y
Received 27 March 2019
Accepted for publication 11 July 2019
Published 26 July 2019 Volume 2019:13 Pages 2553—2563
DOI https://doi.org/10.2147/DDDT.S210228
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Dr Anastasios Lymperopoulos
Purpose: Dydrogesterone (DYG) has been demonstrated to be an alternative progestin in the progestin-primed ovarian stimulation (PPOS) protocol with comparable oocyte retrieval and pregnancy outcomes. However, its safety regarding neonatal outcomes and congenital malformations is still unclear.
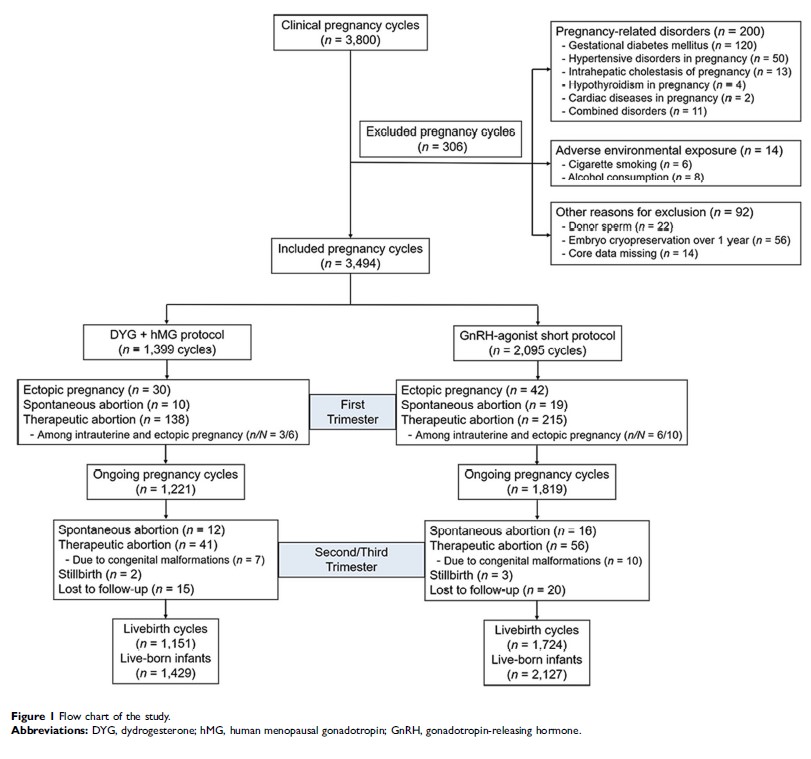
Patients and methods: This retrospective cohort study included 3556 live-born infants after in vitro fertilization and vitrified embryo transfer cycles using the DYG + human menopausal gonadotropin (hMG) protocol (n=1429) or gonadotropin-releasing hormone (GnRH)-agonist short protocol (n=2127) from January 2014 to December 2017. Newborn information was gathered from standardized follow-up questionnaires and/or access to medical records within 7 days after birth. Associations between ovarian stimulation protocols and outcome measures were analyzed by binary logistic regression after adjusting for confounding factors.
Results: In both singletons and twins, birth characteristics regarding mode of delivery, newborn gender, gestational age, birthweight, length at birth and Z-scores were comparable between the two protocols. For adverse neonatal outcomes, the two protocols showed no significant differences on the rates of low birthweight, very low birthweight, preterm birth, very preterm birth, small-for-gestational age, large-for-gestational age and early neonatal death after adjustment. Furthermore, the incidence of major congenital malformations in the DYG + hMG protocol (1.12%) was similar to that in the GnRH-agonist short protocol (1.08%), with the adjusted odds ratio of 0.98 (95% confidence interval [CI]: 0.40–2.39) and 0.90 (95% CI: 0.33–2.41) in singletons and twins, respectively.
Conclusion: Our data suggested that compared with the conventional GnRH-agonist short protocol, application of DYG in the PPOS protocol was a safe option for the newborn population without compromising neonatal outcomes or increasing congenital malformation risks.
Keywords: neonatal outcomes, congenital malformations, dydrogesterone, progestin-primed ovarian stimulation, in vitro fertilization