108985
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

胃癌脊柱转移患者的手术结果和预后因素
Authors Zhong N, Leng A, He S, Yang M, Zhang D, Jiao J, Xu W, Yang X, Xiao J
Received 14 January 2019
Accepted for publication 3 July 2019
Published 24 July 2019 Volume 2019:11 Pages 6971—6979
DOI https://doi.org/10.2147/CMAR.S201372
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Nicola Ludin
Peer reviewer comments 2
Editor who approved publication: Dr Eileen O'Reilly
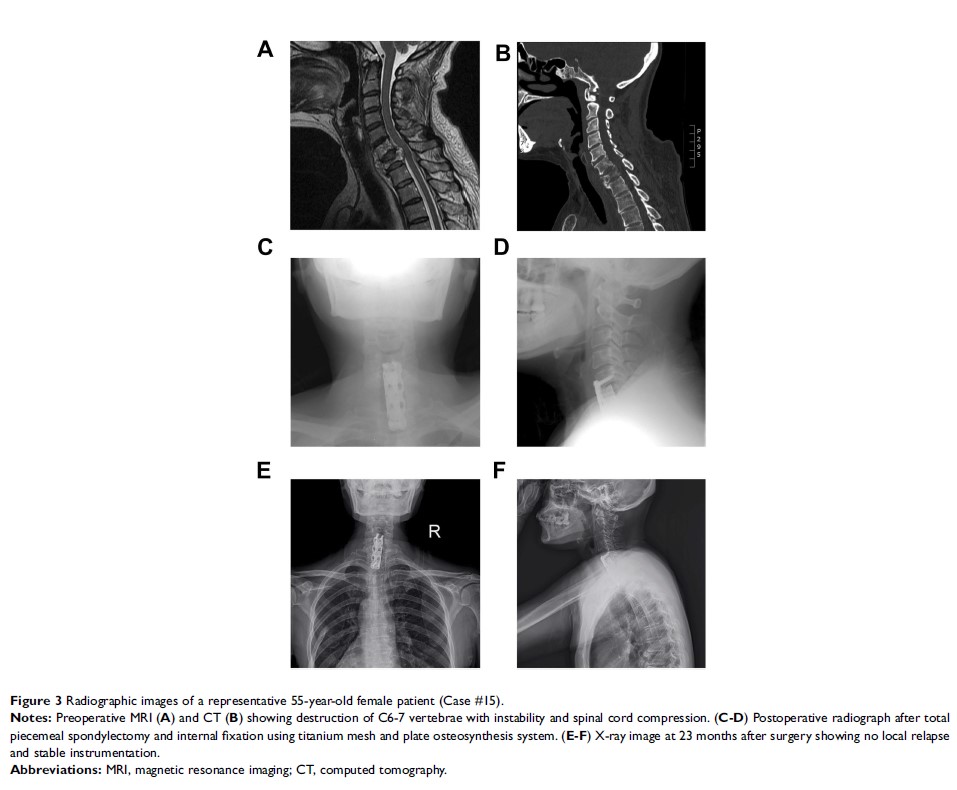
Purpose: To investigate the outcome and prognostic factors of surgery in treating gastric cancer spinal metastasis (GCSM).
Patients and methods: A total of 17 patients with GCSM who have undertaken spinal surgeries have been identified. Kaplan–Meier method and univariate analysis are adopted to investigate the prognostic factors affecting overall survival (OS) and progression-free survival (PFS).
Results: The median PFS and OS are 11.3 months (95% CI: 7.8–14.9 months) and 11.9 months (95% CI: 8.4–15.4 months), respectively. Postoperatively, all patients had substantial pain relief, with mean visual analog scale score descending from 6.6±1.6 to 3.4±1.2. Meanwhile, patients also showed improved neurological functions, with 8 of them having improvements of at least one level in Frankel classification. Univariate analysis presented that patients with carcinoembryonic antigen (CEA)<6 μg/L (p =0.020), lactate dehydrogenase (LDH)<300 U/L (p =0.012), alkaline phosphatase (ALP)<200 U/L (p =0.007), and Tokuhashi score>6 (p =0.027) show longer OS. Moreover, application of bone cement, low level of ALP (<200 U/L), and LDH (<300 U/L) are associated with longer PFS (p <0.05).
Conclusions: Surgery is an efficient option in treating GCSM, due to its efficacy in pain alleviation, function restoration, and stability reconstruction. Low levels of CEA, LDH, ALP, and high Tokuhashi score (>6) are all favorable factors for better OS, whereas low levels of LDH, ALP, and application of bone cement are related with longer PFS.
Keywords: gastric cancer, spine metastasis, surgery