108985
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

精神分裂症患者的抗精神病药物和自然死亡风险
Authors Chen Y, Yang X, Qin X, Yang Q, Fan H, Li J, Song X, Xu S, Guo W, Deng W, Wang Q, Li T, Ma X
Received 28 December 2018
Accepted for publication 4 May 2019
Published 5 July 2019 Volume 2019:15 Pages 1863—1871
DOI https://doi.org/10.2147/NDT.S199748
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Dr Yu-Ping Ning
Background: Research on antipsychotics and early mortality in schizophrenia has arisen from Western countries and results show that mortality from natural causes is obviously increased in schizophrenia. China, differs largely from Western countries in health and social welfare systems, and Asian patients are more susceptible to side-effects and might require less antipsychotics than their Western counterparts. We, therefore, investigated the association between antipsychotic use and increased mortality from natural causes among patients with schizophrenia in China.
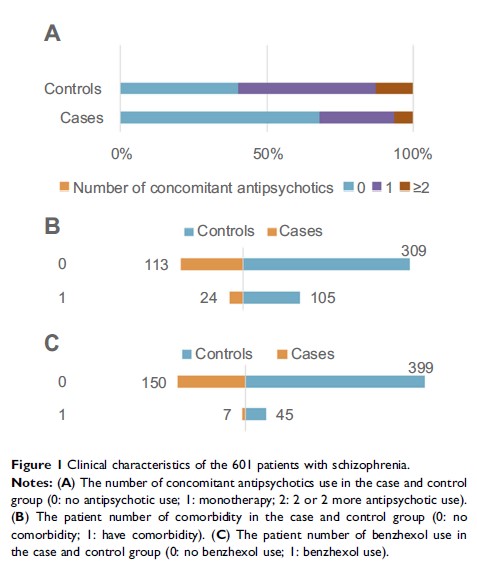
Methods: We conducted a population-based nested case–control study using patients’ hardcopy archives obtained from the Severe Mental Health Disorder Systems of Chengdu between January 1, 2006 and December 31, 2013. We identified all schizophrenic patients aged 18–65 years who died of natural causes in 2013 (N=157), and their age- and gender-matched controls (N=444).
Results: Antipsychotic use was more frequent in controls than in cases (59.9% vs 32.5%). Risk of death decreased significantly in those receiving antipsychotic monotherapy (adjusted odds ratio=0.27, 95% CI=0.16–0.46) and antipsychotic polypharmacy (adjusted odds ratio=0.29, 95% CI=0.12–0.70) than antipsychotic-free patients. Compared with monotherapy, antipsychotic-free treatment was associated with prominently increased mortality (adjusted odds ratio=3.64, 95% CI=2.18–6.08). When stratified by age and gender, the results remained unchanged.
Conclusion: Antipsychotic monotherapy significantly decreased mortality from natural causes in schizophrenic patients while antipsychotic polypharmacy did not contribute to the excess mortality and deserves further clarification. We need to improve the physical health of schizophrenic patients and promote health education among community mental health staff and primary caregivers.
Keywords: antipsychotics, polypharmacy, mortality, odds ratio, schizophrenia