108985
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

血清总胆红素升高可预测接受直接经皮冠状动脉介入治疗的患者 3 年不良后果的高风险
Authors Gao F, Qiang H, Fan XJ, Xue Q, Bai L
Received 30 January 2019
Accepted for publication 8 May 2019
Published 1 July 2019 Volume 2019:15 Pages 811—821
DOI https://doi.org/10.2147/TCRM.S203433
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Cristina Weinberg
Peer reviewer comments 3
Editor who approved publication: Professor Deyun Wang
Purpose: Previous research findings on the association between serum total bilirubin (TB) and cardiovascular events varied with different study populations. Our objective was to clarify the association between serum TB at admission and long-term adverse outcomes in patients with acute coronary syndrome (ACS) and stable angina (SA) undergoing percutaneous coronary intervention (PCI).
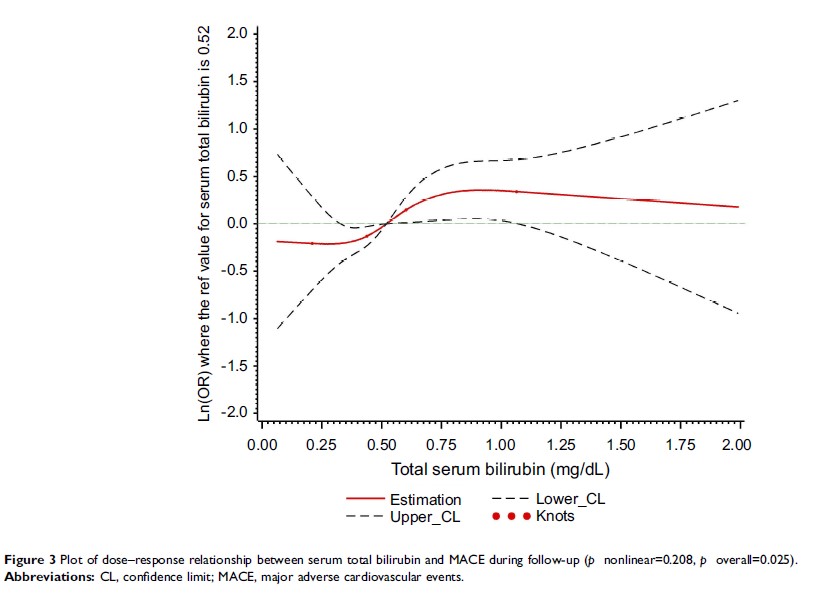
Patients and methods: This prospective cohort study included 2,502 patients who underwent PCI. Information on the study population was obtained from the Dryad Digital Repository. The patients were divided into two groups: high (>0.60 mg/dL) and low TB groups (≤0.60 mg/dL) based on the optimal cutoff value achieved in the receiver operating characteristic curve analysis. The relationships between serum TB at admission and clinical outcomes after PCI were analyzed in multivariable logistic regression models and restricted cubic spline.
Results: In all patients undergoing PCI, TB>0.60 mg/dL was associated with major adverse cardiovascular events (MACE) and cardiovascular death during a 3-year follow-up. The odds ratio (95% confidence interval) was 1.60 (1.22–2.10) and 1.81 (1.22–2.70) for MACE and cardiovascular death, respectively. The association between TB and MACE was not altered by clinical presentation (pfor interaction=0.949).
Conclusion: In patients with ACS and SA undergoing PCI, elevated serum TB was associated with increased risk of MACE and cardiovascular death.
Keywords: bilirubin, acute coronary syndrome, stable angina, primary percutaneous coronary intervention, major adverse cardiovascular; cerebrovascular events