109669
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

已发表论文
危重病人的选择性口咽去污染与选择性消化道去污的对比: 对随机对照试验的一项综合分析
Authors Zhao D, Song J, Gao X, Gao F, Wu Y, Lu Y, Hou K
Published Date July 2015 Volume 2015:9 Pages 3617—3624
DOI http://dx.doi.org/10.2147/DDDT.S84587
Received 14 March 2015, Accepted 21 May 2015, Published 14 July 2015
Background: Selective digestive decontamination (SDD) and selective oropharyngeal
decontamination (SOD) are associated with reduced mortality and infection rates
among patients in intensive care units (ICUs); however, whether SOD has a
superior effect than SDD remains uncertain. Hence, we conducted a meta-analysis
of randomized controlled trials (RCTs) to compare SOD with SDD in terms of
clinical outcomes and antimicrobial resistance rates in patients who were
critically ill.
Methods: RCTs published in PubMed, Embase, and Web of Science were systematically reviewed to compare the effects of SOD and SDD in patients who were critically ill. Outcomes included day-28 mortality, length of ICU stay, length of hospital stay, duration of mechanical ventilation, ICU-acquired bacteremia, and prevalence of antibiotic-resistant Gram-negative bacteria. Results were expressed as risk ratio (RR) with 95% confidence intervals (CIs), and weighted mean differences (WMDs) with 95% CIs. Pooled estimates were performed using a fixed-effects model or random-effects model, depending on the heterogeneity among studies.
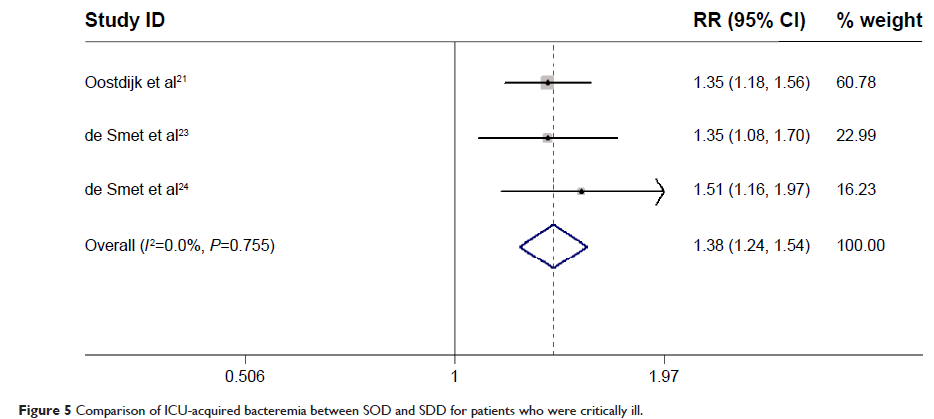
Results: A total of four RCTs involving 23,822 patients met the inclusion criteria and were included in this meta-analysis. Among patients whose admitting specialty was surgery, cardiothoracic surgery (57.3%) and neurosurgery (29.7%) were the two main types of surgery being performed. Pooled results showed that SOD had similar effects as SDD in day-28 mortality (RR =1.03; 95% CI: 0.98, 1.08; P =0.253), length of ICU stay (WMD =0.00 days; 95% CI: -0.2, 0.2; P =1.00), length of hospital stay (WMD =0.00 days; 95% CI: -0.65, 0.65; P =1.00), and duration of mechanical ventilation (WMD =1.01 days; 95% CI: -0.01, 2.02; P =0.053). On the other hand, compared with SOD, SDD had a lower day-28 mortality in surgical patients (RR =1.11; 95% CI: 1.00, 1.22; P =0.050), lower incidence of ICU-acquired bacteremia (RR =1.38; 95% CI: 1.24, 1.54; P =0.000), and lower rectal carriage of aminoglycosides (RR =2.08; 95% CI: 1.68, 2.58; P =0.000), ciprofloxacin-resistant Gram-negative bacteria (RR =1.84; 95% CI: 1.48, 2.29; P =0.000), and respiratory carriage of third-generation cephalosporin-resistant Gram-negative bacteria (RR =2.50; 95% CI: 1.78, 3.5; P =0.000).
Conclusion: SOD has similar effects as SDD in clinical outcomes, but has higher incidence of ICU-acquired bacteremia, and higher carriage of antibiotic-resistant Gram-negative bacteria. However, due to the high cost of SDD and the increased risk of development of antibiotic resistance with the widespread use of cephalosporins in SDD, we would recommend SOD as prophylactic antibiotic regimens in patients in the ICU. More well-designed, large-scale RCTs are needed to confirm our findings.
Keywords: selective digestive decontamination, selective oropharyngeal decontamination, intensive care units, meta-analysis
Methods: RCTs published in PubMed, Embase, and Web of Science were systematically reviewed to compare the effects of SOD and SDD in patients who were critically ill. Outcomes included day-28 mortality, length of ICU stay, length of hospital stay, duration of mechanical ventilation, ICU-acquired bacteremia, and prevalence of antibiotic-resistant Gram-negative bacteria. Results were expressed as risk ratio (RR) with 95% confidence intervals (CIs), and weighted mean differences (WMDs) with 95% CIs. Pooled estimates were performed using a fixed-effects model or random-effects model, depending on the heterogeneity among studies.
Results: A total of four RCTs involving 23,822 patients met the inclusion criteria and were included in this meta-analysis. Among patients whose admitting specialty was surgery, cardiothoracic surgery (57.3%) and neurosurgery (29.7%) were the two main types of surgery being performed. Pooled results showed that SOD had similar effects as SDD in day-28 mortality (RR =1.03; 95% CI: 0.98, 1.08; P =0.253), length of ICU stay (WMD =0.00 days; 95% CI: -0.2, 0.2; P =1.00), length of hospital stay (WMD =0.00 days; 95% CI: -0.65, 0.65; P =1.00), and duration of mechanical ventilation (WMD =1.01 days; 95% CI: -0.01, 2.02; P =0.053). On the other hand, compared with SOD, SDD had a lower day-28 mortality in surgical patients (RR =1.11; 95% CI: 1.00, 1.22; P =0.050), lower incidence of ICU-acquired bacteremia (RR =1.38; 95% CI: 1.24, 1.54; P =0.000), and lower rectal carriage of aminoglycosides (RR =2.08; 95% CI: 1.68, 2.58; P =0.000), ciprofloxacin-resistant Gram-negative bacteria (RR =1.84; 95% CI: 1.48, 2.29; P =0.000), and respiratory carriage of third-generation cephalosporin-resistant Gram-negative bacteria (RR =2.50; 95% CI: 1.78, 3.5; P =0.000).
Conclusion: SOD has similar effects as SDD in clinical outcomes, but has higher incidence of ICU-acquired bacteremia, and higher carriage of antibiotic-resistant Gram-negative bacteria. However, due to the high cost of SDD and the increased risk of development of antibiotic resistance with the widespread use of cephalosporins in SDD, we would recommend SOD as prophylactic antibiotic regimens in patients in the ICU. More well-designed, large-scale RCTs are needed to confirm our findings.
Keywords: selective digestive decontamination, selective oropharyngeal decontamination, intensive care units, meta-analysis