108384
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

糖尿病预测弥漫性大 B 细胞淋巴瘤较低的生存率 - 倾向评分匹配分析
Authors Gao R, Liang JH, Man TS, Wang L, Zhu HY, Wu W, Fan L, Li JY, Yang T, Xu W
Received 25 August 2018
Accepted for publication 11 February 2019
Published 9 April 2019 Volume 2019:11 Pages 2849—2870
DOI https://doi.org/10.2147/CMAR.S185319
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Andrew Yee
Peer reviewer comments 2
Editor who approved publication: Dr Beicheng Sun
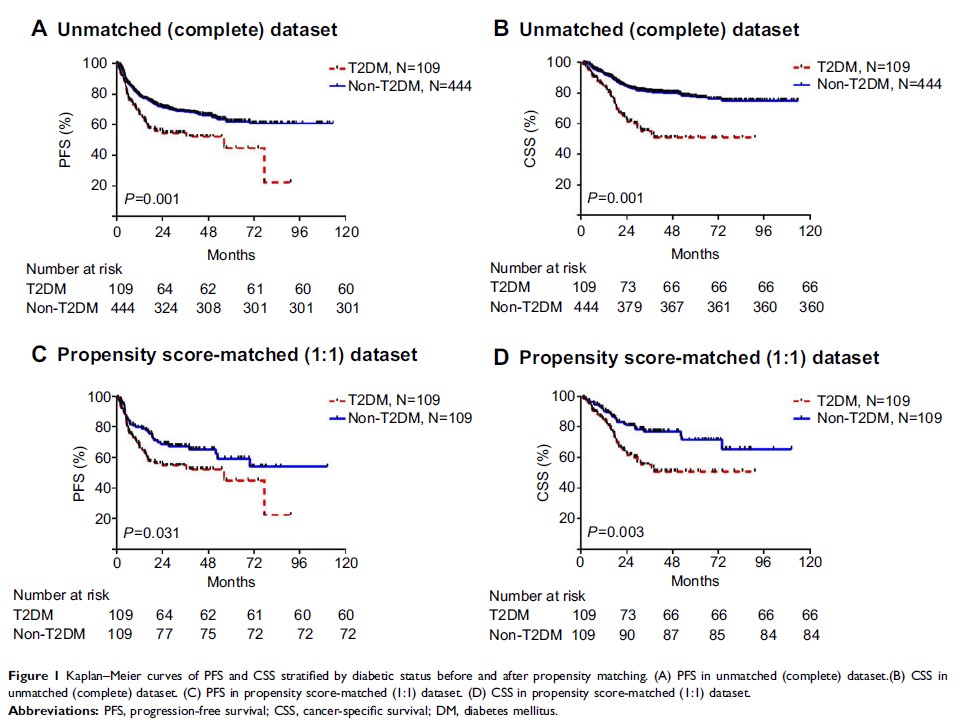
Purpose: Diabetes
mellitus (DM) is associated with elevated cancer risk and poor survival. The
objective of this study was to assess the prognostic value of DM in diffuse
large B-cell lymphoma (DLBCL).
Methods: Five
hundred and fifty-three newly diagnosed DLBCL patients whose treatments
included rituximab were recruited. Propensity score-matched method was
performed to balance baseline characteristics and eliminate possible bias.
Multivariate Cox regression analyses screened the prognostic risk factors in
relation to progression-free survival (PFS) and cancer-specific survival (CSS).
Receiver-operator characteristic curves and the corresponding areas under the
curve (AUC) assessed the predictive accuracy of international prognostic index
(IPI) together with DM.
Results: One
hundred and nine patients (19.71%) had pre-existing DM. In the
propensity-matched cohort, DM was associated with unfavorable PFS and CSS in
rituximab era, and it was an independent risk factor for both inferior PFS and
CSS, especially in patients with age ≤60 years, IPI 0−2, B symptoms and lactate
dehydrogenase ≤upper limit of normal. Prediabetics also demonstrated inferior
prognostic outcomes compared to patients with no diabetic tendency. DM as one
additional point to IPI had larger AUC compared with IPI alone in CSS
prediction and could improve the prognostic capacity of IPI.
Conclusion: The
results indicate that preexisting DM is an important risk factor for survival.
It could help predict life expectancy and build refined prognostication models
for DLBCL.
Keywords: diffuse
large B-cell lymphoma, diabetes mellitus, progression-free survival,
cancer-specific survival, propensity score-matched analysis