108384
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

在 A549 细胞异种移植物裸鼠中由表没食子儿茶素-3-没食子酸酯诱导的血管正常化:与化疗相结合的治疗效果
Authors Deng P, Hu C, Xiong Z, Li Y, Jiang J, Yang H, Tang Y, Cao L, Lu R
Received 16 September 2018
Accepted for publication 25 January 2019
Published 27 March 2019 Volume 2019:11 Pages 2425—2439
DOI https://doi.org/10.2147/CMAR.S187750
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Andrew Yee
Peer reviewer comments 2
Editor who approved publication: Dr Antonella D'Anneo
Purpose: Large-scale studies have revealed that
appropriate antiangiogenic treatment enables the recovery of the normal
structure and function of solid tumor vessels. Epigallocatechin-3-gallate
(EGCG), a natural extract of green tea, has multiple effects on angiogenesis.
However, normalization of blood vessels due to natural ingredients has not yet
been reported. Therefore, we examined the microvasculature, microenvironment,
and efficacy of EGCG combined with chemotherapy in a xenograft model.
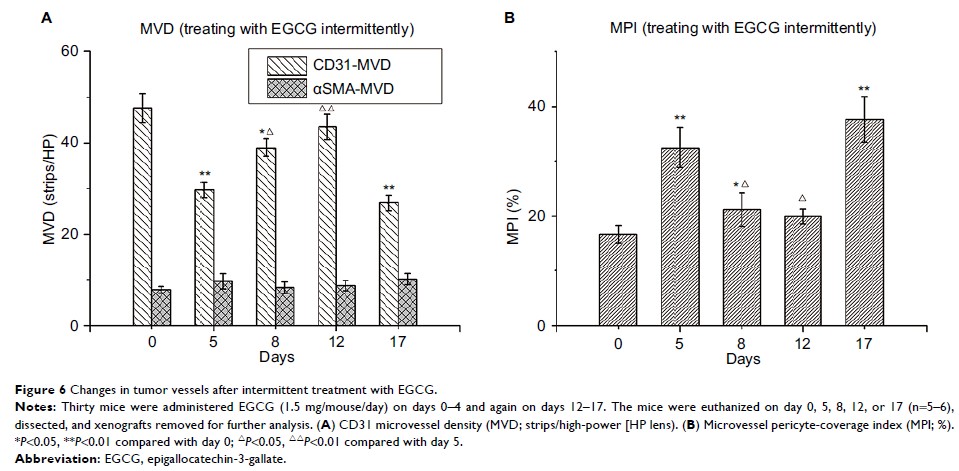
Methods: We
treated A549 cell (human lung adenocarcinoma cell line) xenograft-bearing nude
mice with EGCG in vivo. CD31, αSMA, and collagen IV were labeled and detected
using quantum-dot double-labeled immunofluorescence to measure microvessel
density, microvessel pericyte-coverage index, and collagen IV expression.
Vessel-perfusion function was determined by lectin injection, permeability by
Evans blue extravasation, interstitial fluid pressure using the wick-in-needle
technique, and hypoxia levels using a polarographic electrode and
immunohistochemical pimonidazole labeling. Cisplatin concentration in tumor
tissue was detected using graphite-furnace atomic absorption spectrophotometry.
Xenograft mice were randomized into five groups: treated with saline, cisplatin,
EGCG, EGCG + cisplatin on day 1, or EGCG + cisplatin during the vascular
normalization window. Tumor-growth delay and tumor-suppression rate were
measured to evaluate tumor growth.
Results: EGCG
treatment in vivo caused temporary changes, including transient depression of
microvessel density, microvessel pericyte-coverage index, and collagen IV
expression, transient elevation of vessel perfusion and permeability, and
decreased interstitial fluid pressure and hypoxia. During vascular
normalization, pretreatment with EGCG increased cisplatin concentration in
tumor tissue compared with treatment with cisplatin only. Tumor-growth delay
after treatment in the five groups during the vascular normalization window was
6.3±1.51, 7.5±1.57, 8.3±1.79, 12.1±1.35, and 15.4±1.99 days, indicating
synergistic EGCG–cisplatin effects, especially during the vascular
normalization window (P <0.01).
Conclusion: EGCG-induced
vascular normalization in human lung adenocarcinoma may be a novel modality for
enhancing chemotherapy effects.
Keywords: human
lung adenocarcinoma, EGCG, tumor microenvironment, vascular normalization,
antitumor synergistic effect