108384
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

单一不可治愈因素的晚期胃癌患者前期化疗后行胃切除术的结果:一项队列研究
Authors Li W, Jiang H, Yu Y, Wang Y, Wang Z, Cui Y, Shen K, Shen Z, Fang Y, Liu T
Received 29 October 2018
Accepted for publication 22 January 2019
Published 5 March 2019 Volume 2019:11 Pages 2007—2013
DOI https://doi.org/10.2147/CMAR.S192570
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Andrew Yee
Peer reviewer comments 2
Editor who approved publication: Dr Ahmet Emre Eskazan
Purpose: Chemotherapy
is the standard care for patients with incurable advanced gastric cancer.
Whether or when the addition of gastrectomy to chemotherapy improves survival
of advanced gastric cancer patients with a single noncurable factor remains
controversial. We aimed to evaluate the superiority of gastrectomy following
chemotherapy vs chemotherapy alone regarding overall survival (OS) in these
patients.
Patients and methods: Patients
with advanced gastric cancer from January 2008 to December 2014 were retrieved
from our prospectively acquired database and retrospectively analyzed. The
patients with a single noncurable factor were grouped in terms of cancer
treatment: chemotherapy alone or gastrectomy following chemotherapy.
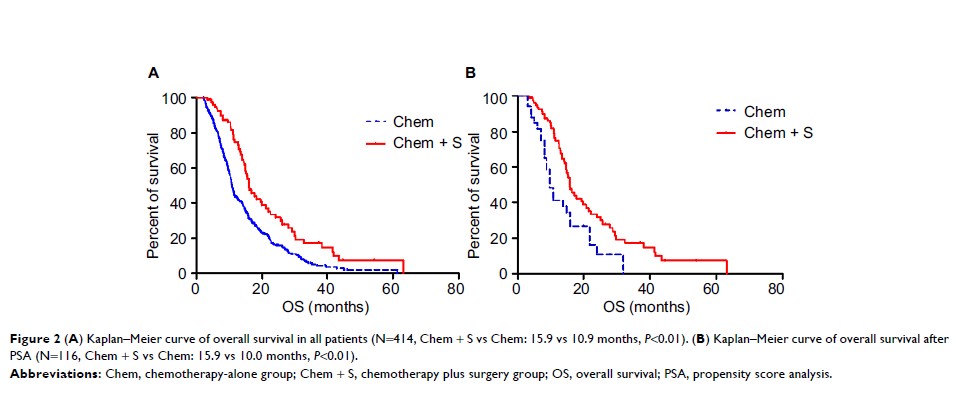
Results: Four
hundred and fourteen patients (333 chemotherapy alone and 81 gastrectomy
following chemotherapy) were included in this study. Kaplan–Meier survival
curve showed a significant difference on median OS between chemotherapy-alone
group and the gastrectomy plus chemotherapy group (10.9 vs 15.9 months, P <0.01). After
propensity score analysis (n=126), chemotherapy plus surgery (81 patients) also
showed survival benefit over chemotherapy alone (35 patients) (15.9 vs 10.0
months, P <0.01).
Furthermore, stratified analyses indicated that patients with liver metastasis,
Conclusion: This
study suggests that gastrectomy after chemotherapy could lead to survival
benefit over chemotherapy alone in advanced gastric cancer patients with a
single nonresectable factor if the disease was controllable by chemotherapy.
Keywords: gastric
cancer, palliative surgery, overall survival, propensity score analysis