108899
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

PD-1/PD-L1 免疫检查点抑制剂用于转移性膀胱癌治疗的有效性和安全性的荟萃分析
Authors Fan Z, Liang Y, Yang X, Li B, Cui L, Luo L, Jia Y, Wang Y, Niu H
Received 3 September 2018
Accepted for publication 13 January 2019
Published 4 March 2019 Volume 2019:12 Pages 1791—1801
DOI https://doi.org/10.2147/OTT.S186271
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Cristina Weinberg
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Geoffrey Pietersz
Background: This
article is a meta-analysis aiming to systematically assess the efficacy and
safety profiles of PD-1/PD-L1 inhibitors in patients with advanced or
metastatic bladder cancer.
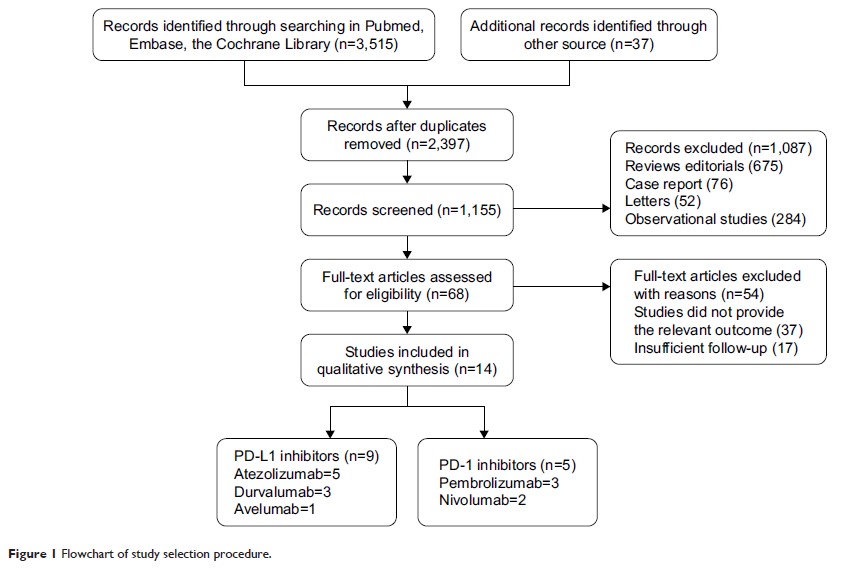
Methods: We
extracted and examined data from phase I, II, and III clinical trials from the
Medline, Embase, and the Cochrane Library, which included patients with
metastatic bladder cancer who were treated with PD-1/PD-L1 inhibitors. We
performed a meta-analysis to investigate several indexes of efficacy and
safety, including the objective response rate (ORR), 1-year overall survival
(OS) rate, 1-year progression-free survival (PFS) rate, and adverse event (AE)
rate of immune checkpoint inhibitors. The material data were calculated and
pooled using The R Project for Statistical Computing and Review Manager 5.3.
Results: After
excluding ineligible records, 14 clinical trials were included in our analysis.
The pooled frequencies of all-grade AEs and grade ≥3 AEs were 0.63 (95% CI
0.61–0.65, P =0.34)
and 0.14 (95% CI 0.11–0.17, P =0.0072), respectively. The summary ORR was 0.21 (95%
CI 0.18–0.24 P =0.07), and the 1-year OS and 1-year PFS rates were
0.48 (95% CI 0.42–0.54 P =0.0013) and 0.21 (95% CI 0.16–0.26 P =0.04), respectively.
The OR of ORR between the PD-L1-positive and -negative groups was 3.09 (95% CI
2.01–4.75, P =0.08).
Conclusion: The
PD-1/PD-L1 therapy showed appropriate efficacy and acceptable incidence of
treatment-related AEs. In addition, the level of discrimination of PD-L1
expression might be related to the effect of the PD-1/PD-L1 inhibitors, and
patients displaying positive expression might experience a better curative
effect than patients displaying negative expression.
Keywords: PD-1
inhibitor, PD-L1 inhibitor, immunotherapy, metastatic bladder cancer,
meta-analysis, bladder cancer, oncology