108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

Impact of a probiotic-based hospital sanitation on antimicrobial resistance and HAI-associated antimicrobial consumption and costs: a multicenter study
Authors Caselli E, Arnoldo L, Rognoni C, D'Accolti M, Soffritti I, Lanzoni L, Bisi M, Volta A, Tarricone R, Brusaferro S, Mazzacane S
Received 15 November 2018
Accepted for publication 25 January 2019
Published 27 February 2019 Volume 2019:12 Pages 501—510
DOI https://doi.org/10.2147/IDR.S194670
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Dr Joachim Wink
Purpose: Antimicrobial resistance (AMR) is one of
the major threats to human health, and the high frequency of resistant
pathogens in the hospital environment can contribute to the transmission of
difficult-to-treat health care-associated infections (HAIs). We recently
reported that, compared with conventional chemical cleaning, the use of a
microbial-based sanitation strategy (Probiotic Cleaning Hygiene System [PCHS])
was associated with remodulation of hospital microbiota and reduction of HAI
incidence. Here, we aimed to analyze the impact of PCHS on AMR and related
effects, such as HAI-associated antimicrobial drug consumption and costs.
Patients and methods: Five Italian hospitals, enrolled in a multicenter study where
conventional sanitation methods were replaced with PCHS, were included in the
analysis. The study period included a 6-month observation for each sanitation
type. Surface microbiota AMR was analyzed using microarray, nested PCR,
antibiogram, and microdilution tests. Drug consumption data and related costs
were obtained from the medical records of all hospitalized patients affected by
HAIs.
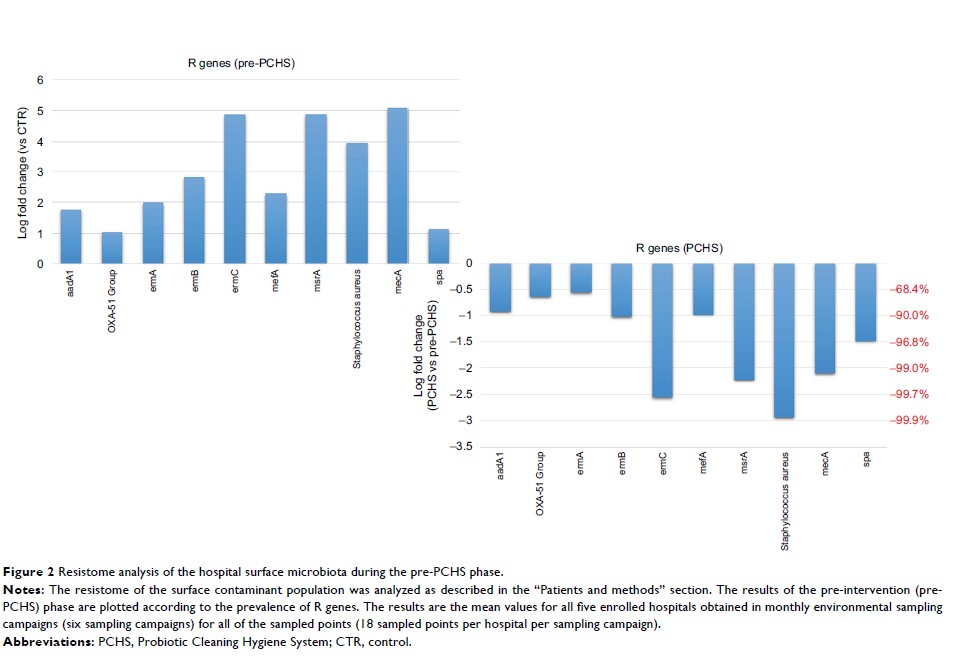
Results: PCHS
use was associated with up to 99% decrease of the AMR genes harbored by surface
hospital microbiota, independently of the resistance types originally present
in each individual setting (Pc <0.01).
Functional assays confirmed the molecular data, demonstrating a 33%–100%
decrease of resistant strains depending on the antibiotic type. Antimicrobial
drug consumption associated with HAI onset showed a global 60.3% decrease, with
a 75.4% decrease of the associated costs.
Conclusion: The
spread of AMR in the hospital environment can be limited by the use of
sanitation methods to remodulate the hospital microbiota, leading to lower
antimicrobial consumption and costs. This approach might be considered as part
of broader infection prevention and control strategies.
Keywords: AMR,
HAI, antimicrobials, drug consumption, costs