108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

在血液疾病中广泛耐药的革兰氏阴性细菌血流感染
Authors Zhou L, Feng S, Sun G, Tang B, Zhu X, Song K, Zhang X, Lu H, Liu H, Sun Z, Zheng C
Received 19 October 2018
Accepted for publication 18 January 2019
Published 26 February 2019 Volume 2019:12 Pages 481—491
DOI https://doi.org/10.2147/IDR.S191462
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 3
Editor who approved publication: Professor Suresh Antony
Background: Extensively
drug-resistant Gram-negative bacterial (XDR-GNB) bloodstream infection (BSI) is
difficult to treat and is associated with a high mortality rate in patients
with hematological diseases. The aim of this study is to investigate the
predisposing risk factors and the efficacy of the antibiotic treatment in these
patients, including exploration of efficacy and adverse effects of high-dose
tigecycline.
Methods: Between
January 2013 and December 2017, 27 XDR-GNB BSI patients with hematological
diseases were diagnosed and retrospectively reviewed in the current study.
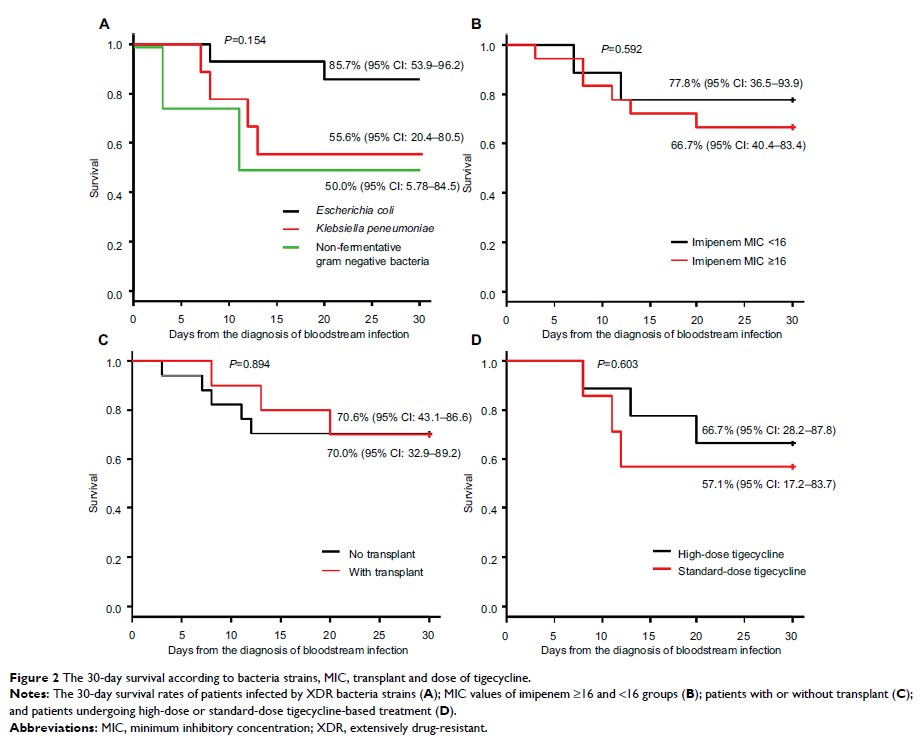
Results: Clinical
response in patients with severe complications (such as severe neutropenia
>10 days, grade III–IV acute graft-versus-host disease (aGVHD), and
concurrent pneumonia) was significantly lower than in patients without or with
only mild complications (P =0.033). The efficacy rate was 62.5% (10/16) in
patients with tigecycline-based combination therapy regimen, 77.8% (7/9) with a
high-dose tigecycline regimen, and 42.9% (3/7) with a standard-dose tigecycline
regimen (P =0.36).
The 30-day survival rates of patients undergoing high-dose or standard-dose
tigecycline treatment were 66.7% (95% CI: 28.2–87.8) and 57.1% (95% CI:
17.2–83.7), respectively, (P =0.603). Patients with mild complications were
associated with superior 30-day survival rates than patients with severe
complications (93.8% vs 36.4%, P =0.001), >10 days of neutropenia (90.9% vs
33.3%, P =0.012),
severe aGVHD (100% vs 40%, P =0.049), and concurrent pneumonia (84.6% vs
57.1%, P =0.048).
Conclusion: Our study
indicated that XDR-GNB BSI in patients of hematological diseases with severe
complications, such as long duration of neutropenia (>10 days) and severe
aGVHD were associated with poor clinical response and short survival. We first
indicated that these patients undergoing high-dose tigecycline treatment had an
improved clinical response and an increased 30-day survival rate compared with
the standard-dose group, although the differences were not statistically
significant. This might be due to more severe complicated patients enrolled in
high-dose group and the limited number size in our study.
Keywords: carbapenem
resistant bacterial infection, bloodstream infection, high-dose tigecycline,
hematological malignancies