108384
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

骨密度与乳腺癌风险之间的关系:10 项队列研究的系统评价和剂量反应荟萃分析
Authors Chen JH, Yuan Q, Ma YN, Zhen SH, Wen DL
Received 20 September 2018
Accepted for publication 5 January 2019
Published 13 February 2019 Volume 2019:11 Pages 1453—1464
DOI https://doi.org/10.2147/CMAR.S188251
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 3
Editor who approved publication: Dr Antonella D'Anneo
Purpose: The
evidence from recent epidemiological studies investigating the relationship
between bone mineral density (BMD) and the risk of breast cancer (BC) remains
inconsistent.
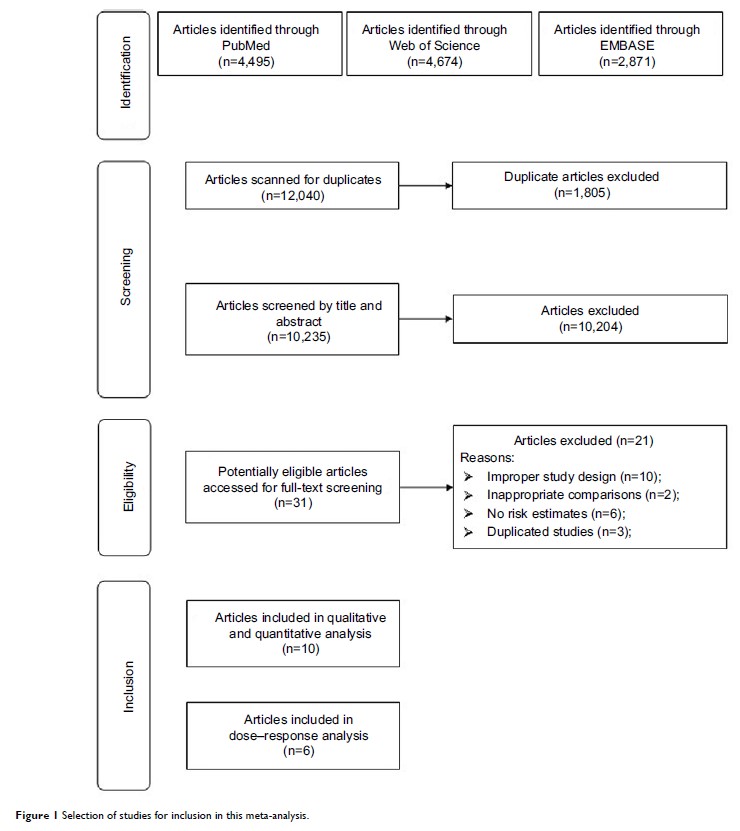
Materials and methods: The
PubMed, EMBASE, and Web of Science databases were comprehensively searched by
two independent authors to identify related cohort studies from the inception
of the databases through January 31, 2018. Similarly, two researchers
separately extracted the data from the selected studies, and any differences
were resolved by discussion. Summarized relative risks (RRs) and 95% CIs were
summarized via inverse variance weighted random-effects meta-analysis.
Heterogeneity among studies was assessed with the I 2 statistic.
Results: Ten
studies with 1,522 BC patients among 81,902 participants were included in this
meta-analysis. Compared to the participants with the lowest BMD at the lumbar
spine, those with the highest BMD had a significantly lower RR for BC (RR =0.75;
95% CI =0.60–0.93; I 2=23.0%). In the subgroup analyses, although the
directions of the results were consistent with those of the main findings, not
all showed statistical significance. We failed to detect an association between
BMD at the femoral neck or total hip and the risk of BC (RR =0.94; 95% CI
=0.66–1.33; I 2=72.5%). Furthermore, the results of the
dose–response analysis did not show a significant association between BMD at
the lumbar spine, femoral neck, or total hip and the risk of BC. Funnel plot
and statistical analyses showed no evidence of publication bias.
Conclusion: There is
no relationship between BMD and the risk of BC. More prospective cohort studies
are warranted to further investigate this issue.
Keywords: bone
mineral density, breast cancer, cohort studies, meta-analysis, risk