108384
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

对胸腰椎骨质疏松性椎体压缩骨折而言,经皮椎体成形术后进行支撑是无效的
Authors Zhang J, Fan Y, He X, Du J, Hao D
Received 30 October 2018
Accepted for publication 11 January 2019
Published 5 February 2019 Volume 2019:14 Pages 265—270
DOI https://doi.org/10.2147/CIA.S192821
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Justinn Cochran
Peer reviewer comments 3
Editor who approved publication: Dr Zhi-Ying Wu
Objective: The
objective of this study was to evaluate the effectiveness of bracing after
percutaneous vertebroplasty (PVP) for thoracolumbar osteoporotic vertebral
compression fractures (OVCF).
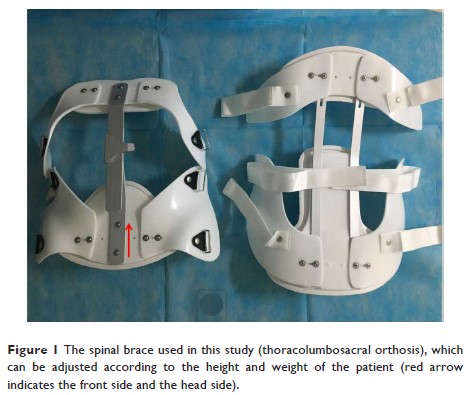
Methods: This is a
retrospective study where we recruited 138 patients with single-level
thoracolumbar OVCF who underwent PVP from January 2018 to March 2018 without
bracing after PVP (Group A). The visual analog score (VAS) and vertebral body
compression ratio (VCR) were recorded at preoperation, on the second day, at 2
weeks, 1 month, and 6 months after operation. Oswestry Disability Index (ODI)
was recorded at preoperation, 2 weeks, 1 month, and 6 months after operation.
Propensity score matching identified 138 historical patients (Group B) as
controls, who used rigid brace for 3 weeks after the surgery, from January 2017
to December 2017 using six independent variables (preoperation): age, sex, VAS,
ODI, bone mineral density, and body mass index. The indicators and
complications were compared between the two groups.
Results: Compared
with preoperation, VAS and VCR were significantly improved (P <0.05) in both
groups on the second day after operation. At 2 weeks, 1 month, and 6 months
after PVP operation, ODI, VAS, and VCR were all significantly improved than at
preoperation (P <0.05).
There were no statistical differences between the two groups in VAS and VCR on
the second day, at 1 month and 6 months after PVP (P >0.05). There
were no significant differences between Groups A and B in ODI at 2 weeks and 6
months after operation (P >0.05) but ODI for Group B at 1 month after
operation was significantly higher than Group A (P <0.05). Eleven
cases in Group A and 13 cases in Group B had poor pain relief on the second day
after operation, and there were no significant differences in VAS and ODI
between the two subgroups at 2 weeks, 1 month, and 6 months after PVP. There
were no significant differences in the collapse and refracture rates between
the two groups.
Conclusion: In
summary, in terms of quality of life and complications after operation,
postoperative bracing did not result in improved outcomes. Presence or absence
of bracing did not relieve postoperative residual pain. In contrast, bracing
for 3 weeks after operation reduced the quality of life in the short term.
Keywords: percutaneous
vertebroplasty, osteoporotic vertebral compression fractures, brace