108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

Utilization of pain medications and its effect on quality of life, health care utilization and associated costs in individuals with chronic back pain
Authors Desai R, Hong YR, Huo J
Received 11 September 2018
Accepted for publication 17 December 2018
Published 1 February 2019 Volume 2019:12 Pages 557—569
DOI https://doi.org/10.2147/JPR.S187144
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Dr Michael Schatman
Purpose: Pain
medications are widely prescribed to treat chronic back pain (CBP). However,
the effect of using pain medications on individuals with CBP has received very
little attention.
Objective: The aim
of this study was to determine the patterns of pharmacological treatment in the
population with CBP and assess its impact on quality of life, health care
utilization and associated costs in USA.
Patients and methods: Retrospective,
cross-sectional data obtained from the Medical Expenditure Panel Survey (MEPS),
from 2011 to 2015, were utilized for this study. Pharmacological treatment for
CBP was categorized into three mutually exclusive categories: 1) opioids only,
2) nonsteroidal anti-inflammatory drugs (NSAIDs) only, 3) opioids and NSAIDs
(combination). The effect of the use of these treatments was also evaluated.
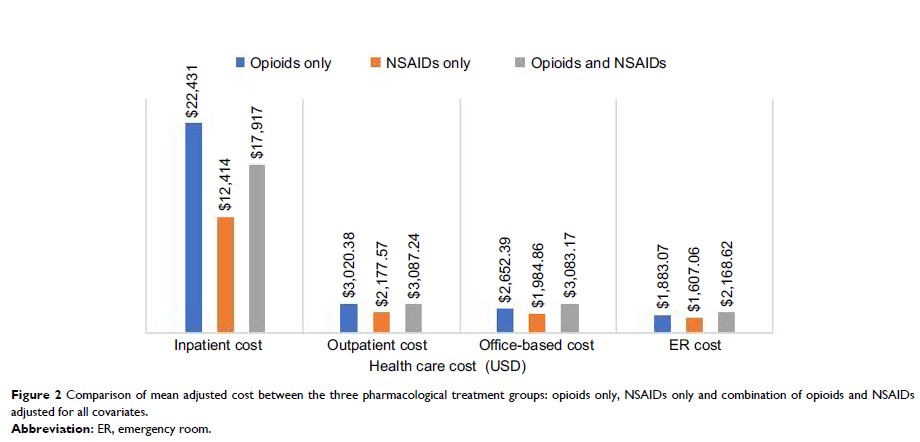
Results: A total
of 5,203 individuals with CBP were identified. Of these, 2,568 (49.4%) utilized
opioids only, 1,448 (27.8%) utilized NSAIDs only and 1,187 (22.8%) utilized
both pain medications. Lower health-related quality-of-life scores on both the
Short Form Health Survey-12 version 2 (SF-12v2) components (mental component
summary score: 44.42 vs 46.67, P <0.001; physical component summary score: 35.34 vs
40.11, P <0.001)
were observed for the opioid-only group compared to the NSAID-only group. In
addition, individuals utilizing opioids only had greater utilization of
inpatient services, office-based services, outpatient services and emergency
room visits along with higher related health care costs.
Conclusion: Future
researchers need to investigate the long-term risks and benefits of opioids,
and policy makers should evaluate the prescribing guidelines to aim for a more
patient-centered care.
Keywords: opioids,
NSAIDs, quality of life, health care resource utilization, cost