108384
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

IB 期非小细胞肺癌手术患者术前血小板与淋巴细胞比值和淋巴细胞与单核细胞比值的预后意义
Authors Chen Y, Wang W, Zhang X, Yu X, Xi K, Wen Y, Wang G, Feng X, Zhang L
Received 15 June 2018
Accepted for publication 19 September 2018
Published 8 November 2018 Volume 2018:10 Pages 5411—5422
DOI https://doi.org/10.2147/CMAR.S177320
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Andrew Yee
Peer reviewer comments 3
Editor who approved publication: Dr Beicheng Sun
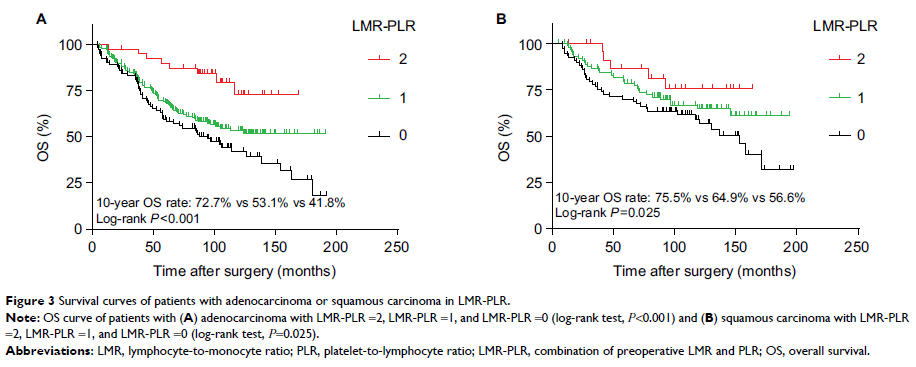
Background: Research indicates that the presence of a systemic inflammatory
response plays an important role in predicting survival in patients with
cancer. The aim of this study was to investigate the prognostic value of
preoperative neutrophil-to-lymphocyte ratio (NLR), lymphocyte-to-monocyte ratio
(LMR), platelet-to-lymphocyte ratio (PLR), prognostic nutritional index, and
the combination of preoperative LMR and PLR (LMR-PLR) in predicting the
survival of patients with stage IB non-small-cell lung cancer (NSCLC).
Materials and methods: We retrospectively analyzed clinical data of 577
patients with stage IB NSCLC who underwent pneumonectomy from January 1999 to
December 2009. Univariate and multivariate Cox survival analyses were used to
evaluate the prognostic indicators, including LMR-PLR. The cutoff values for
LMR and PLR were defined by the receiver operating characteristic (ROC) curve
analysis. According to the ROC curve, the recommended cutoff values of LMR and
PLR were 3.16 and 81.07, respectively. We divided the patients into three groups
according to their LMR and PLR status and defined them with different scores.
Patients with both high LMR (>3.16) and low PLR (≤81.07) were given a score
of 2, whereas those with one or neither were scored 1 or 0, respectively.
Survival curves were plotted using the Kaplan–Meier method and compared with
the log-rank test. Cox proportional hazards analyses were used to identify the
factors associated with overall survival (OS).
Results: The median follow-up time was 93.77 months. The
allocation of the LMR-PLR score was as follows: LMR-PLR = 0, 193 (33.4%)
patients; LMR-PLR = 1, 308 (53.4%) patients; and LMR-PLR = 2, 76 (13.2%)
patients. After multivariate analysis, our results showed that LMR-PLR was an
independent prognostic indicator for OS (P =0.001). The
10-year OS rates were 70.0%, 60.4%, and 49.5% for LMR-PLR =2, LMR-PLR =1, and
LMR-PLR =0, respectively (P <0.001).
Conclusion: This study demonstrated that preoperative LMR and PLR
are simple, readily available, and low-cost biomarkers. Preoperative LMR-PLR
score can be used as a valuable prognostic marker for long-term survival in
stage IB NSCLC patients who underwent surgery.
Keywords: IB
non-small-cell lung cancer, platelet-to-lymphocyte ratio,
lymphocyte-to-monocyte ratio, prognostic factors, systemic inflammation,
pneumonectomy