108384
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

乳腺癌亚型及初次诊断时远处转移的风险:一个基于人口的研究
Authors Xiao W, Zheng S, Yang A, Zhang X, Zou Y, Tang H, Xie X
Received 10 June 2018
Accepted for publication 23 August 2018
Published 5 November 2018 Volume 2018:10 Pages 5329—5338
DOI https://doi.org/10.2147/CMAR.S176763
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Dr Beicheng Sun
Background: It was unclear whether breast cancer subtypes are associated with the
risk of site-specific metastases. This study aimed to evaluate the relationship
between molecular subtypes and distant metastatic sites and their prognostic
significance.
Methods: We identified 295,213 patients with invasive breast cancer from 2010 to
2014 using the Surveillance, Epidemiology and End Results database. Subtypes
were classified into four categories: hormone receptor (HR+)/human epidermal growth factor receptor 2 (HER2−), HR+/HER2+, HR−/HER2+, and triple-negative (HR−/HER2−). Logistic regression
was used to assess the association between metastasis location and subtypes.
Multivariate Cox models were used to estimate the overall survival (OS) of
related factors.
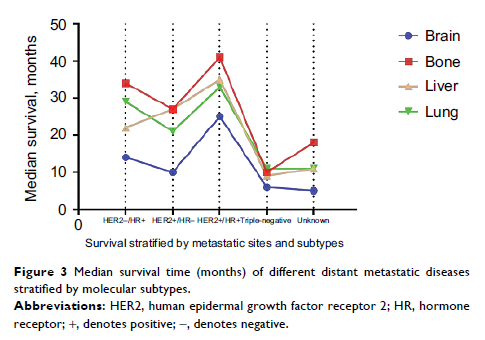
Results: According to our study, 3.28%, 1.52%, 1.20%, and 0.35% of newly
diagnosed breast cancers presented bone, lung, liver, and brain metastases at
diagnosis, respectively. Both metastatic sites and subtypes significantly
affected the OS after metastasis. In multivariate analysis, HR+/HER2+ subtype (OR as compared
with HR+/HER2− subtype, 1.30 [95% CI, 1.22–1.39]) significantly correlated with
elevated bone metastasis risk, whereas HR−/HER2+ did not. Both
HER2+ subtypes (HR+/HER2+ and HR−/HER2+) were significantly
associated with higher rates of liver, brain, and lung metastases, while the
highest OR was observed in liver metastases. Triple-negative tumors had a
higher rate of brain (OR, 1.95 [95% CI, 1.61–2.35]), liver (OR, 1.35 [95% CI,
1.20–1.51]), and lung metastases (OR, 1.34 [95% CI, 1.21–1.47]), but a
significantly lower rate of bone metastases (OR, 0.64 [95% CI, 0.59–0.69]) than
HR+/HER2− tumors.
Conclusions: Breast cancer subtypes are associated with different metastatic
patterns and confer different prognostic impacts. Molecular subtypes can
identify patients at increased risk of site-specific metastases.
Keywords: breast cancer, molecular subtypes, metastasis behavior, prognosis,
metastatic sites