109669
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

手术切除脑转移瘤和对中国非小细胞肺癌 (NSCLC) 患者的原发肿瘤的根治性治疗的预后
Authors Li Z, Zhang X, Jiang X, Guo C, Sai K, Yang Q, He Z, Wang Y, Chen Z, Li W, Mou Y
Published Date April 2015 Volume 2015:8 Pages 855—860
DOI http://dx.doi.org/10.2147/OTT.S80329
Received 5 January 2015, Accepted 13 February 2015, Published 16 April 2015
Purpose: Brain
metastasis is the most common complication of brain cancer; nevertheless,
primary lung cancer accounts for approximately 20%–40% of brain metastases
cases. Surgical resection is the preferred treatment for brain metastases.
However, no studies have reported the outcome of surgical resection of brain
metastases from non–small-cell lung cancer (NSCLC) in the People’s Republic of
China. Moreover, the optimal treatment for primary NSCLC in patients with
synchronous brain metastases is hitherto controversial.
Patients and methods: We
retrospectively analyzed the cases of NSCLC patients with brain metastases who
underwent neurosurgical resection at the Sun Yat-sen University Cancer Center,
and assessed the efficacy of surgical resection and the necessity of aggressive
treatment for primary NSCLC in synchronous brain metastases patients.
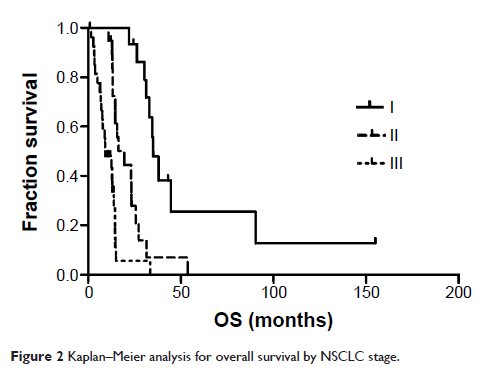
Results: A total of 62
patients, including 47 men and 15 women, with brain metastases from NSCLC were
enrolled in the study. The median age at the time of craniotomy was 54 years
(range 29–76 years). At the final follow-up evaluation, 50 patients had died.
The median OS time was 15.1 months, and the survival rates were 70% and 37% at
1 and 2 years, respectively. The median OS time of synchronous brain metastases
patients was 12.5 months. Univariate analysis revealed that radical treatment
of primary NSCLC was positively correlated with survival, and it was an
independent prognostic factor in the multivariate analysis.
Conclusion: Surgical resection
is an effective treatment for brain metastases. Besides craniotomy, radical
therapy is necessary for the management of primary NSCLC in patients with
synchronous brain metastases.
Keywords: synchronous brain
metastases, neurosurgery, whole-brain radiation therapy