108552
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

Maternal depression and antidepressant use during pregnancy and the risk of autism spectrum disorder in offspring
Authors Hagberg KW, Robijn AL, Jick S
Received 18 July 2018
Accepted for publication 18 September 2018
Published 1 November 2018 Volume 2018:10 Pages 1599—1612
DOI https://doi.org/10.2147/CLEP.S180618
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Justinn Cochran
Peer reviewer comments 5
Editor who approved publication: Professor Henrik Toft Sørensen
Background: Results of some studies suggest that prenatal antidepressant
exposure increases the risk of autism spectrum disorder (ASD) in offspring,
while other studies suggest that depression independently increases the risk of
having a child with ASD. Thus, confounding by indication is a concern.
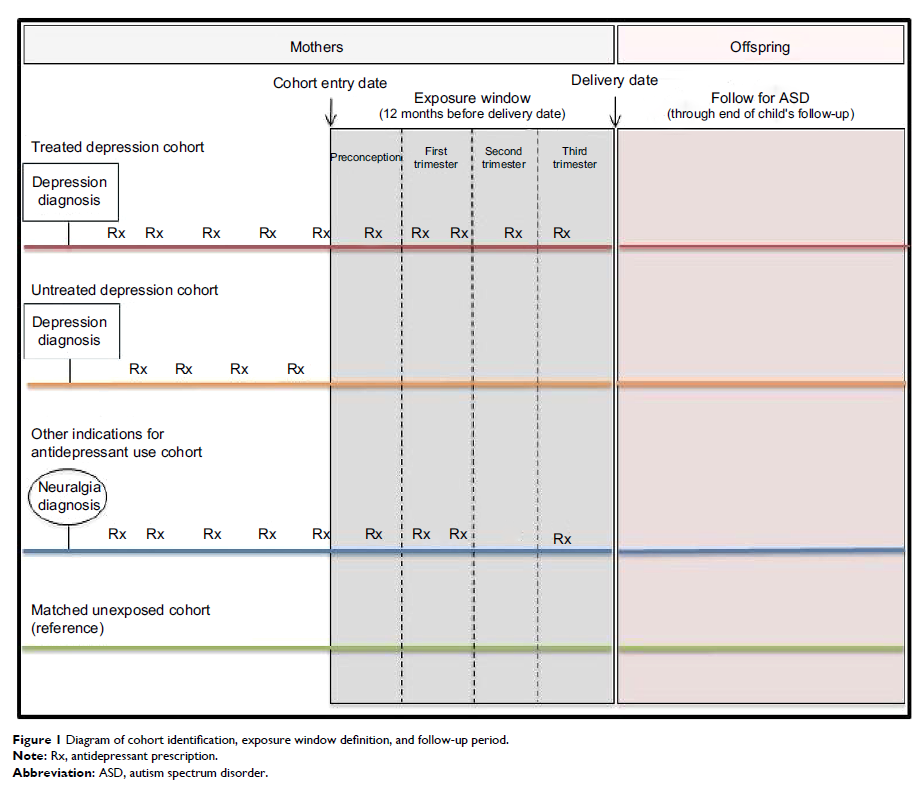
Objective: The aim of this study was to estimate the risk of ASD in offspring
of women who were exposed to antidepressants and/or had depression during
pregnancy compared to unexposed women.
Materials and
methods: We conducted a cohort study with
nested sibling case–control analysis. Using the UK Clinical Practice Research
Datalink (CPRD), we identified mother–baby pairs where the mother had ≥12
months of history before the delivery date and the child had ≥3 years of
follow-up. Exposures during pregnancy were classified as 1) depression treated
with antidepressants, 2) untreated depression, 3) other indications for
antidepressant use, and 4) 4:1 match of unexposed women with no history of
depression or antidepressant use. We calculated the prevalence of ASD and
relative risk (RR) with 95% CI. In the sibling analysis, we compared exposure
among ASD cases to that of non-ASD siblings born to the same mother. We
calculated ORs and 95% CIs for women with treated and untreated depression,
compared to unexposed.
Results: We identified 2,154 offspring with ASD among 194,494 mother–baby
pairs. Compared to unexposed, the RR of ASD was 1.72 (95% CI 1.54–1.93) for
treated depression and 1.50 (95% CI 1.28–1.75) for untreated depression, while
the RR was not elevated in women who received antidepressants for other
indications (RR =0.73, 95% CI 0.41–1.29). Additional analyses to assess the
effects of severity of depression suggest that the risk of ASD in offspring
increases with increasing severity, not with the antidepressant treatment. The
results of the sibling analysis were similar to the main analysis.
Conclusion: Women with depression during pregnancy have an increased risk of
having a child with ASD, regardless of antidepressant use.
Keywords: depression, pregnancy, antidepressants, autism, autism spectrum
disorder