108552
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

衍生的中性粒细胞与淋巴细胞比率对三阴性乳腺癌手术预后的价值
Authors Ren K, Yin Y, He F, Shao Y, Wang S
Received 18 July 2018
Accepted for publication 12 September 2018
Published 24 October 2018 Volume 2018:10 Pages 4891—4898
DOI https://doi.org/10.2147/CMAR.S180695
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Amy Norman
Peer reviewer comments 3
Editor who approved publication: Dr Antonella D'Anneo
Introduction: The role of derived neutrophil-to-lymphocyte ratio (dNLR) in
predicting the prognosis of patients with triple-negative breast cancer (TNBC)
has not been well studied. Here, we attempted to investigate the significance
of dNLR in predicting the prognosis of patients with surgical (nonmetastatic)
TNBC.
Methods: A total of 281 patients diagnosed with surgical TNBC in The First
Affiliated Hospital of University of Science and Technology of China from
February 2005 to March 2015 were retrospectively included in this study.
Kaplan–Meier curve analysis was used to assess the disease-free survival (DFS)
and overall survival (OS). We used Cox regression model to assess the
prognostic significance of pretreatment dNLR and other clinicopathological
parameters in TNBC patients.
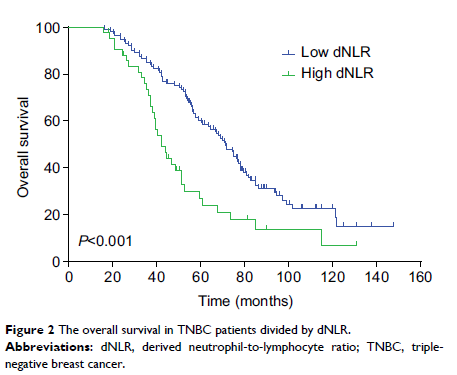
Results: The median DFS in TNBC patients who had low dNLR and high dNLR was
28.9 and 15.1 months (P <0.001),
respectively, whereas the median OS in patients who had low dNLR and high dNLR
was 71.2 and 42.3 months (P <0.001),
respectively. In patients aged ≤50 years and with invasive ductal
carcinoma, a low dNLR predicted better DFS and OS compared with a high dNLR.
Multivariate analysis demonstrated that the increased dNLR was a risk factor of
poor DFS (HR=1.90, 95% CI: 1.52–2.46, P =0.007) and OS
(HR=2.56, 95% CI: 1.69–3.58, P =0.001).
Conclusion: Pretreatment dNLR is an independent factor of prognosis for TNBC
patients, which potentially allows clinical doctors to improve outcomes of
patients with high dNLR by treating with aggressive therapy, such as high-dose adjuvant
chemotherapy and radiotherapy.
Keywords: dNLR, TNBC, inflammation, immunity, prognosis