108552
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

上海市儿科患者碳青霉烯类耐药肺炎克雷伯菌的耐药表型及临床分子流行病学研究
Authors Tian D, Pan F, Wang C, Sun Y, Zhang H
Received 28 May 2018
Accepted for publication 2 August 2018
Published 24 October 2018 Volume 2018:11 Pages 1935—1943
DOI https://doi.org/10.2147/IDR.S175584
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Cristina Weinberg
Peer reviewer comments 3
Editor who approved publication: Dr Joachim Wink
Background: Carbapenem-resistant Klebsiella pneumoniae (CRKP)
has caused wide global disseminations and serious clinical outcomes in
pediatric patients, and the purpose of this study was to analyze drug
resistance, molecular epidemiology, and clinical characteristics of CRKP from
children in Shanghai, China.
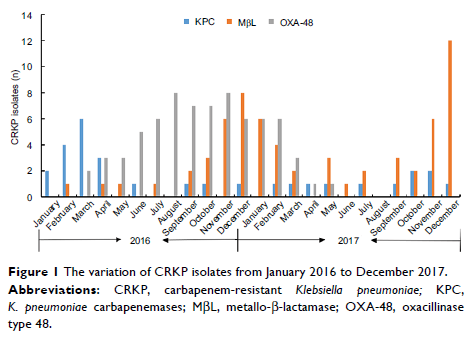
Methods: A retrospective study was conducted from January 2016 to December
2017, and a total of 170 CRKP isolates were collected. Antimicrobial
susceptibility was determined by the broth microdilution method. MAST D73C and
polymerase chain reaction were used for the analysis of carbapenemase types.
Multilocus sequence typing of K. pneumoniae was
performed for genetic relationship. Clinical data were also reviewed.
Results: Of the 170 CRKP isolates, blaOXA-232 was mainly detected with a proportion of 42.35%, followed by blaNDM-1 (20.59%), blaKPC-2 (17.65%), blaNDM-5 (16.47%), and blaIMP-4 (1.18%). The predominant gene was blaOXA-232 in 2016 (54.46%; 55/101) and blaNDM-1 in 2017 (31.88%; 22/69). All these 170 CRKP isolates showed high
resistance to cephalosporins and carbapenems (>95%), except for tigecycline
and colistin. Sixteen distinct sequence types were observed with ST15 being
mostly identified (41.76%). Most CRKP harboring OXA-232 type carbapenemase
belonged to ST15, while NDM-1 type belonged to ST37 and KPC-2 type belonged to
ST11. Furthermore, other β-lactamase genes including blaTEM , blaCTX-M , and DHA-1 were also found in this study. Clinical data reviewed that
more than half of the patients produced clinical infections (112/170), mainly
lower respiratory tract (58/112) and bloodstream (21/112) infections. A
majority of these children had received therapy of antibiotics before CRKP
isolation, especially for carbapenems (76/170) and β-lactam/β-lactamase
inhibitor combinations (91/170).
Conclusions: Our data revealed the increasing incidence of
OXA-232-producing K. pneumoniae from
pediatric patients in Shanghai, and infection control measures should be
conducted to limit the spread of CRKP strains.
Keywords: Klebsiella pneumoniae ,
carbapenemases, drug resistance, OXA-232, NDM-5, children