108384
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

五年中国医院侵入性真菌监测网(CHIF-NET)关于非蟾蜍酵母引起的侵袭性真菌感染的研究:物种分布和唑类易感性
Authors Xiao M, Chen SCA, Kong F, Fan X, Cheng JW, Hou X, Zhou ML, Wang H, Xu YC
Received 11 May 2018
Accepted for publication 10 August 2018
Published 9 October 2018 Volume 2018:11 Pages 1659—1667
DOI https://doi.org/10.2147/IDR.S173805
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Dr Eric Nulens
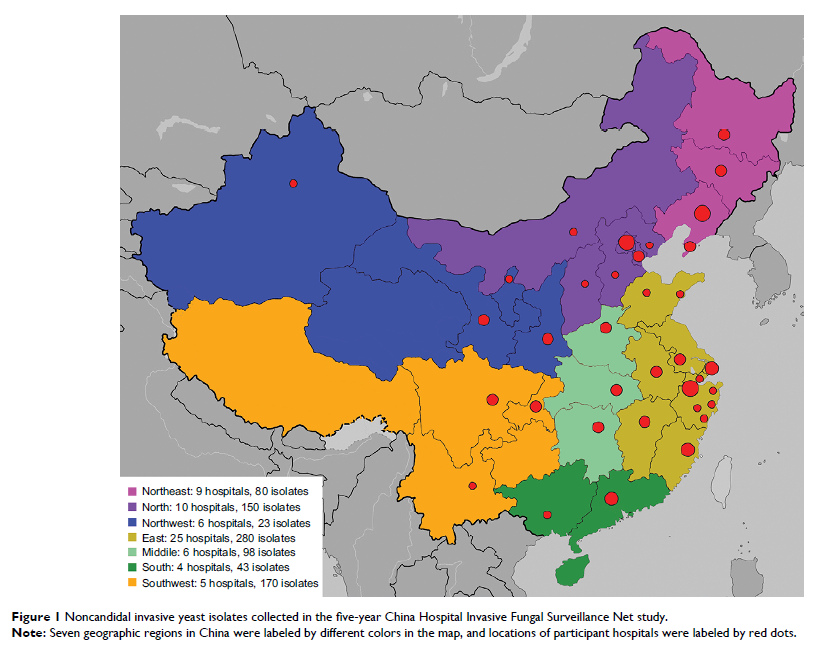
Purpose: In this study, we report results from a 5-year surveillance for noncandidal yeast species causing invasive infections from 65 hospitals in China.
Materials and methods: Species identification was carried out by matrix-assisted laser desorption/ionization-time of flight mass spectrometry (MALDI-TOF MS) supplemented by rDNA sequencing, and fluconazole and voriconazole susceptibilities of yeasts were determined by Clinical and Laboratory Standards Institute (CLSI) disk diffusion methods.
Results: Overall, 884 noncandidal isolates belonging to 38 species were collected. Cryptococcus neoformans was the most common (75.6%), which also comprised 96.5% of the isolates from cerebrospinal fluid (CSF) and 62.6% from blood, followed by Trichosporon asahii (6.9%) and Rhodotorula mucilaginosa (5.1%). Fluconazole susceptibility and resistant rates were 74.1% and 9.7% for C. neoformans and 81.0% and 5.2% for T. asahii . Voriconazole exhibited good activity in comparison to these two species (99.5% and 98.3% of the isolates, were susceptible). However, 100% of the R. mucilaginosa isolates were resistant to both azoles. Other noncandidal yeast species showed reduced susceptibility to fluconazole (53.3%) but most were susceptible to voriconazole (94.3%). Over the 5 years, a decrease in the proportion of fluconazole-susceptible isolates was observed for C. neoformans (90%–67%, P <0.001) and other noncandidal yeast species (91%–66%, P <0.001). Moreover, the prevalence of azole-resistant R. mucilaginosa increased from 1% to 7% (P <0.001).
Conclusion: The shift in azole susceptibilities in mainland China calls for continued surveillance for noncandidal yeasts.
Keywords: invasive fungal infections, noncandidal yeasts, epidemiology, azole susceptibility, China