108384
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

中国三个地区接受拉米夫定抗逆转录病毒治疗的 705 名艾滋病病毒感染者的 HBV 感染特征
Authors Su M, Liao L, Xing H, Wang S, Li Y, Lu W, He L, Deng J, Shao Y, Li T, Zhuang H
Received 11 May 2018
Accepted for publication 3 July 2018
Published 2 October 2018 Volume 2018:11 Pages 1635—1644
DOI https://doi.org/10.2147/IDR.S173757
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
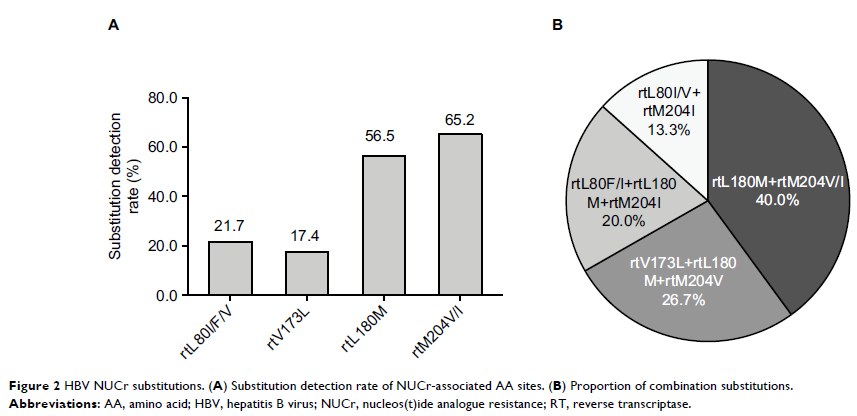
Purpose: This study aimed to investigate the HIV and hepatitis B virus
(HBV) co-infection in three HIV high endemic areas with different modes of HIV
transmission and explore the HBV nucleos(t)ide analogue resistance (NUCr)
substitutions in this cohort receiving antiretroviral therapy (ART).
Patients and
methods: The enrolled 705 HIV-infected
patients were from three different regions in China and received
lamivudine-based ART for at least 1 year. After screening for hepatitis B
surface antigen (HBsAg), the hepatitis B e antigen (HBeAg), and antibody
against hepatitis B core antigen (anti-HBc and anti-HBc IgM), HBV DNA in plasma
of patients positive for HBsAg was tested. The reverse transcriptase (RT)
sequences of HBV were analyzed by direct sequencing.
Results: The overall HBsAg-positive rate was 7.1% (50/705) (Guangxi
[25/170, 14.7%], Xinjiang [13/257, 5.1%], and Henan [12/278, 4.3%]). The age,
transmission route, and ethnic status were found to be associated with HIV/HBV
co-infection. We obtained 23 HBV RT sequences belonging to genotypes B (9/23,
39.1%), C (13/23, 56.5%), and D (1/23, 4.4%). About 65.2% (15/23) of RT
sequences harbored NUCr substitutions, all of which had combination
substitution patterns. Patients with HBV NUCr had significantly higher HBV DNA
level and ratio of HBeAg-positive than those without NUCr. None of the patients
was found to have both lamivudine-resistant HBV and HIV.
Conclusion: Our results suggested that HBsAg-positive rate in the studied
patients was similar to that of the general population in each of the studied
regions, where the age, transmission route, and ethnic status might also play
roles in HIV/HBV co-infection. The HBV combination NUCr substitutions were
common in co-infected patients under ART. Monitoring of HBV infection and NUCr
substitutions in HIV-infected patients would help in providing better clinical
decisions and management, thus lowering patients’ risks to develop end-stage
liver diseases.
Keywords: human immunodeficiency virus, hepatitis B virus, co-infection,
nucleos(t)ide analogue resistance, hepatitis B surface antigen