108384
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

较低的中性粒细胞与淋巴细胞比率预测医院获得性肺炎患者多药耐药性铜绿假单胞菌感染的高风险
Authors Zhou YQ, Feng DY, Li WJ, Yang HL, Wang ZN, Zhang TT, Chen ZG
Received 5 July 2018
Accepted for publication 24 August 2018
Published 2 October 2018 Volume 2018:14 Pages 1863—1869
DOI https://doi.org/10.2147/TCRM.S179181
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Professor Deyun Wang
Background and
purpose: Hospital-acquired pneumonia (HAP)
remains an important cause of morbidity and mortality despite advances in
antimicrobial therapy. The emergence of multidrug resistant (MDR) Pseudomonas aeruginosa (PA)
is of major concern. Our aim was to evaluate the risk factors and prognosis of
HAP due to MDR-PA infection.
Patients and methods: In a retrospective observational study, we collected data on all
episodes of HAP caused by PA (PA-HAP) occurring from January 2013 to December
2016. Characteristics of patients with drug-sensitive PA were compared with
those with MDR-PA. Data of demographic, underlying conditions, peripheral
neutrophil-to-lymphocyte ratio (NLR), and clinical outcomes were collected and
analyzed.
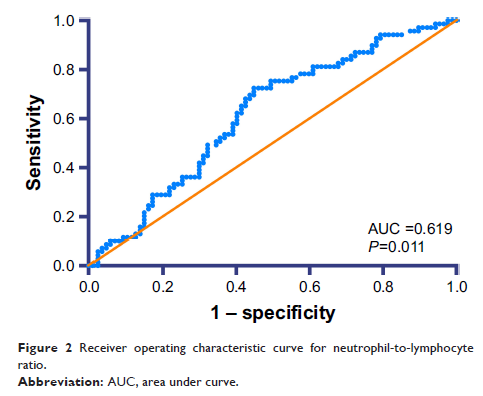
Results: One hundred fifty-seven patients with PA-HAP were included, of
which 69 (43.9%) patients were diagnosed with MDR-PA infection. There were
significant differences between MDR-PA group and non-MDR-PA group on the
following variables: initial inappropriate antibiotic therapy (P <0.001, OR 0.103, 95% CI
0.044–0.244), admission in more than two departments in previous 30 days (P <0.001, OR 0.186, 95% CI
0.072–0.476), and NLR level (P =0.020, OR 0.911,
95% CI 0.843–0.985). The effect of antibiotic treatment was significantly
different (P <0.001, OR 4.263, 95% CI
2.142–8.483). The 30-day mortality was higher in MDR-PA group than that in
non-MDR-PA group (P <0.001).
Conclusion: We have shown that lower NLR level was identified as a clinical
predictor of MDR-PA infection in HAP patients. Even with goal-directed therapy,
MDR-PA infection implicates poor outcomes in patients with HPA.
Keywords: risk factors, prognosis, multidrug-resistant Pseudomonas aeruginosa ,
hospital-acquired pneumonia