108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

对 COPD 患者支气管进行光学相干断层扫描评估,用肺功能检查和脉冲示波法肺功能和脉冲示波法检测小气道疾病的意义
Authors Su ZQ, Guan WJ, Li SY, Ding M, Chen Y, Jiang M, Chen XB, Zhong CH, Tang CL, Zhong NS
Received 29 April 2018
Accepted for publication 17 July 2018
Published 1 October 2018 Volume 2018:13 Pages 3031—3044
DOI https://doi.org/10.2147/COPD.S172639
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Justinn Cochran
Peer reviewer comments 2
Editor who approved publication: Professor Chunxue Bai
Background: Spirometry confers limited value for identifying small-airway
disorders (SADs) in early-stage COPD, which can be detected with impulse
oscillometry (IOS) and endobronchial optical coherence tomography (EB-OCT).
Whether IOS is useful for reflecting small-airway morphological abnormalities
in COPD remains unclear.
Objectives: To compare the diagnostic value of spirometry
and IOS for identifying SADs in heavy-smokers and COPD based on the objective
assessment with EB-OCT.
Methods: We recruited 59 COPD patients (stage I, n=17;
stage II, n=18; stage III–IV, n=24), 26 heavy-smokers and 21 never-smokers.
Assessments of clinical characteristics, spirometry, IOS and EB-OCT were
performed. Receiver operation characteristic curve was employed to demonstrate
the diagnostic value of IOS and spirometric parameters.
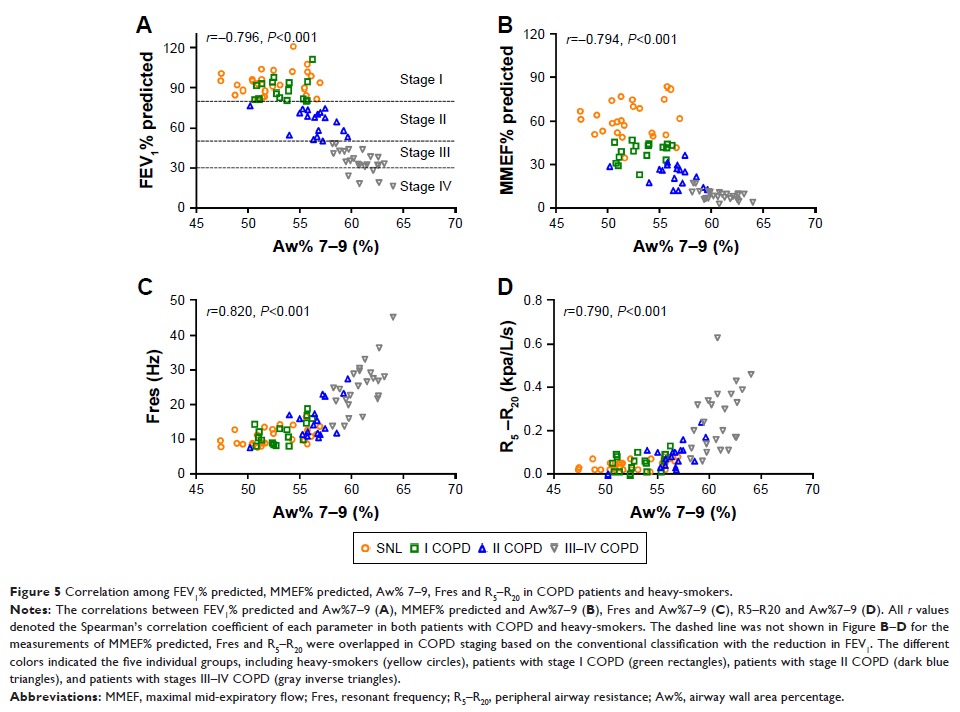
Results: More advanced staging of COPD was associated
with greater abnormality of IOS and spirometric parameters. Resonant frequency
(Fres) and peripheral airway resistance (R5–R20) conferred greater diagnostic values than forced
expiratory volume in one second (FEV1%) and maximal
(mid-)expiratory flow (MMEF%) predicted in discriminating SADs in never-smokers
from heavy-smokers (area under curve [AUC]: 0.771 and 0.753 vs 0.570 and 0.558,
respectively), and heavy-smokers from patients with stage I COPD (AUC: 0.726
and 0.633 vs 0.548 and 0.567, respectively). The combination of IOS (Fres
and R5–R20) and
spirometric parameters (FEV1% and MMEF%
predicted) contributed to a further increase in the diagnostic value for
identifying SADs in early-stage COPD. Small airway wall area percentage (Aw%
7–9), an EB-OCT parameter, correlated significantly with Fres and R5–R20 in COPD
and heavy-smokers, whereas EB-OCT parameters correlated with FEV1% and MMEF% in advanced, rather than early-stage,
COPD.
Conclusions: IOS parameters correlated with the degree of
morphologic abnormalities of small airways assessed with EB-OCT in COPD and
heavy-smokers. Fres and R5–R20 might be sensitive parameters that reliably
reflect SADs in heavy-smokers and early-stage COPD.
Keywords: chronic
obstructive pulmonary disease, optical coherence tomography, diagnostic value,
impulse oscillometry, small airway disorder