108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

睡眠发作潜伏期与失眠老年人骨密度降低有关:一项回顾性研究
Authors Tong Q, Wu WZ, Wu Q, Yu YB, Lv XL, Wang BZ, Wang GF
Received 8 January 2018
Accepted for publication 25 June 2018
Published 30 August 2018 Volume 2018:13 Pages 1525—1530
DOI https://doi.org/10.2147/CIA.S161922
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Dr Wu
Purpose: Inconsistent outcome about association between insufficient sleep and bone mineral density (BMD) has been reported. The present study aimed to determine whether BMD was associated with score of Pittsburgh Sleep Quality Index (PSQI).
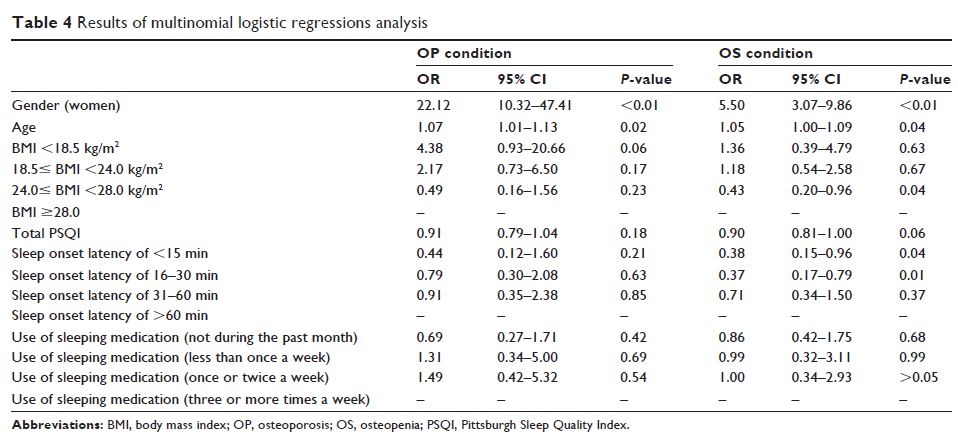
Methods: A total of 410 patients (mean age 81.6±5.9 years) attending our hospital for evaluation of sleep were retrospectively studied. Dual-Energy X-ray Absorptiometry was used to measure BMD and T-score at femoral neck and lumbar spines over L2–L4 regions. Subjective sleep status was evaluated by the PSQI questionnaires. The Mann–Whitney U test and chi-square analysis were used to compare continuous variables and categorical variables, respectively. Spearman correlation test was conducted to find the relationship between BMD and other clinical factors. Multinomial logistic regressions analysis was performed to analyze independent factors predicting BMD.
Results: Majority of the participants with osteoporosis (OP) were female and had lower body mass index (BMI) and higher sleep onset latency score. Spearman correlation test showed that gender, BMI, score of total PSQI, and sleep onset latency were significantly related to BMD and T-score in femoral neck and lumbar region L2–L4. Finally, multinomial logistic regression analysis demonstrated that gender and age were independent factors for OP and osteopenia and that after adjustment for gender, age, and BMI, sleep onset latency of <15 minutes (OR: 0.38; 95% CI: 0.15–0.96; P =0.04) and 16–30 minutes (OR: 0.37; 95% CI: 0.17–0.79; P =0.01) were less likely to have reduced BMD.
Conclusion: There was a significant association between BMD and sleep onset latency, suggesting that, in elderly patients with sleep problem, BMD measurement and intervention for OP might be valuable.
Keywords: bone mineral density, insomnia, osteoporosis, osteopenia, Pittsburgh Sleep Quality Index, sleep onset latency