108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

产生广谱 β-内酰胺酶的碳青霉烯类耐药肠杆菌科细菌感染的流行病学和危险因素:一项双病例对照研究的结果
Authors Tian X, Sun S, Jia X, Zou H, Li S, Zhang L
Received 9 May 2018
Accepted for publication 18 July 2018
Published 29 August 2018 Volume 2018:11 Pages 1339—1346
DOI https://doi.org/10.2147/IDR.S173456
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 4
Editor who approved publication: Professor Suresh Antony
Purpose: Carbapenem-resistant Enterobacteriaceae (CRE) have been increasingly reported worldwide and pose a serious public threat, but the clinical significance of extended-spectrum β-lactamase (ESBL) production in CRE is not well established.
Patients and methods: A retrospective case–case–control study was conducted to identify the clinical characteristics of patients with ESBL-CRE. The susceptibility of isolates obtained from these patients was assessed. The detection of ESBL and carbapenemase-related genes was performed by PCR methods. Predictors of 30-day mortality in patients with ESBL-CRE infection were also identified in our study.
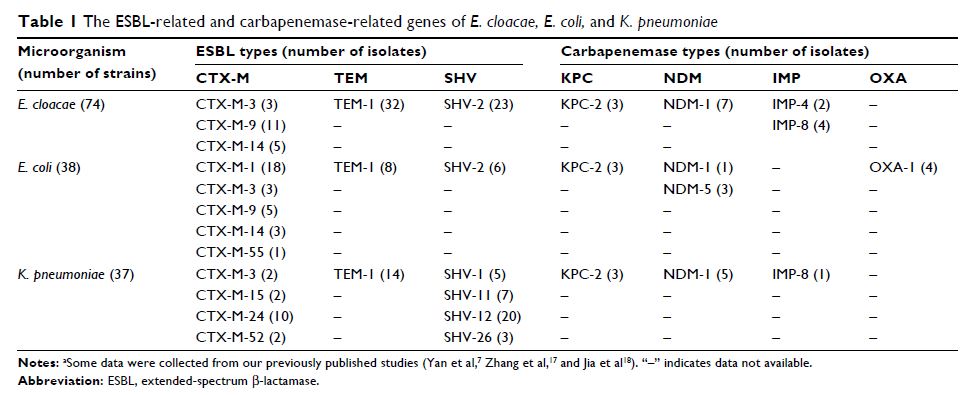
Results: A total of 149 patients with CRE infection caused by Enterobacter cloacae (n=74), Escherichia coli (n=38), and Klebsiella pneumoniae (n=37) were identified in Chongqing, Southwestern China, between January 2011 and December 2014. Of the 35 isolates detected with carbapenemase-related genes, 16 isolates had New Delhi metallo-β-lactamase (NDM), nine isolates had K. pneumoniae carbapenemase (KPC), seven isolates had imipenemase (IMP), and four isolates had oxacillinase (OXA)-1. One strain of enterobacter cloacae carried both NDM-1 and IMP-8 genes. ESBL isolates included the genes CTX-M (72/149), SHV (64/149), and TEM (54/149). All ESBL-CRE isolates exhibited ertapenem resistance, and the rate of cephalosporin resistance was relatively high in general. Independent risk factors for infection with ESBL-CRE included previous exposure to β-lactam antibiotics, transfer from another hospital, and some underlying diseases. In addition, solid tumors, hypoalbuminemia, and central venous catheters were independent predictors of mortality in patients with ESBL-CRE infection.
Conclusion: Physicians should understand the peculiar predictors for the identification of these organisms among high-risk patients.
Keywords: risk factors, carbapenem, resistance, ESBL, mortality