108384
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

臭氧大自血疗法联合药物治疗带状疱疹后神经痛的影响及安全性
Authors Hu B, Zheng J, Liu Q, Yang Y, Zhang Y
Received 14 October 2017
Accepted for publication 20 June 2018
Published 27 August 2018 Volume 2018:11 Pages 1637—1643
DOI https://doi.org/10.2147/JPR.S154154
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 3
Editor who approved publication: Dr Michael Schatman
Introduction: We investigated the effect and safety of ozone autohemotherapy combined with pharmacological therapy in postherpetic neuralgia (PHN).
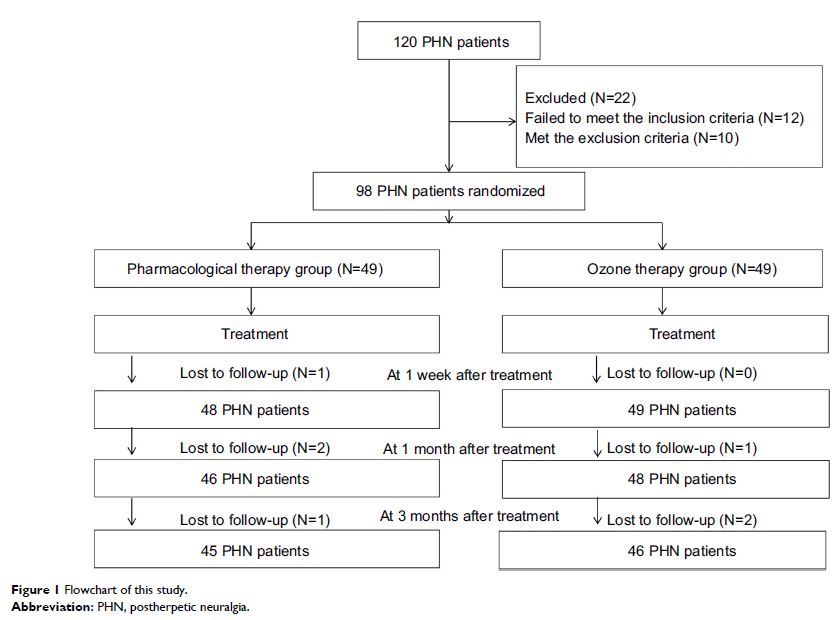
Methods: Ninety-eight patients with PHN were enrolled in this study and randomly divided into a pharmacological therapy group and ozone autohemotherapy group (49 patients in each group). The PHN patients in the pharmacological therapy group were administered pharmacological therapy for 2 weeks, whereas PHN patients in the ozone autohemotherapy group were given ozone autohemotherapy (200 mL blood from patients, the concentration of medical ozone was set as 30 μg/mL using an ozone medical apparatus, 40 mL medical ozone was incubated in 200 mL autologous blood for 3–5 minutes) combined with pharmacological therapy for 2 weeks. The Visual Analog Scale (VAS), the 50% VAS reduction in the initial value, McGill Pain Questionnaire (MPQ), the Patients’ Global Impression of Change (PGIC) scale, and the World Health Organization Quality of Life (WHOQOL-BREF) instrument were used to evaluate the outcomes of all PHN patients before therapy and at 1 week, 1 month, and 3 months after therapy.
Results: Forty-five patients in the pharmacological therapy group and 47 patients in the ozone autohemotherapy group completed the study. Compared with before therapy, the two groups showed significant improvements in VAS, MPQ, PGIC, and WHOQOL-BREF scores after therapy (P <0.05). Moreover, compared with the scores of the pharmacological therapy group, the ozone autohemotherapy group’s scores were significantly improved in the VAS, MPQ, PGIC, and WHOQOL-BREF as well as the 50% VAS reduction of the initial value after therapy (P <0.05). Finally, there were no statistically significant differences in adverse effects between groups after therapy (P >0.05).
Conclusion: The results of this study demonstrated that ozone autohemotherapy combined with pharmacological therapy was superior to isolated pharmacological therapy in patients with PHN and was an effective and safe way to relieve PHN.
Keywords: ozone autohemotherapy, pharmacological therapy, clinical trial, postherpetic neuralgia