108384
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

腹腔镜肝切除术治疗老年结直肠癌肝转移患者的近期和远期疗效
Authors Yue M, Li S, Yan G, Li C, Kang Z
Received 7 November 2017
Accepted for publication 14 March 2018
Published 10 August 2018 Volume 2018:10 Pages 2581—2587
DOI https://doi.org/10.2147/CMAR.S156379
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Lucy Goodman
Peer reviewer comments 3
Editor who approved publication: Professor Luzhe Sun
Purpose: This study aimed to evaluate the short- and long-term outcomes of
laparoscopic hepatectomy (LH) for colorectal liver metastases (CRLM) in elderly
patients.
Patients and
methods: Between January 2009 and January
2016, LH was performed for 241 consecutive patients who were ≥60 years old and
had CRLM. Based on their age at the LH, the patients were divided into an
elderly group (≥70 years old, 78 patients) and a middle-aged group (60–69 years
old, 163 patients). The short- and long-term outcomes were compared between the
two groups.
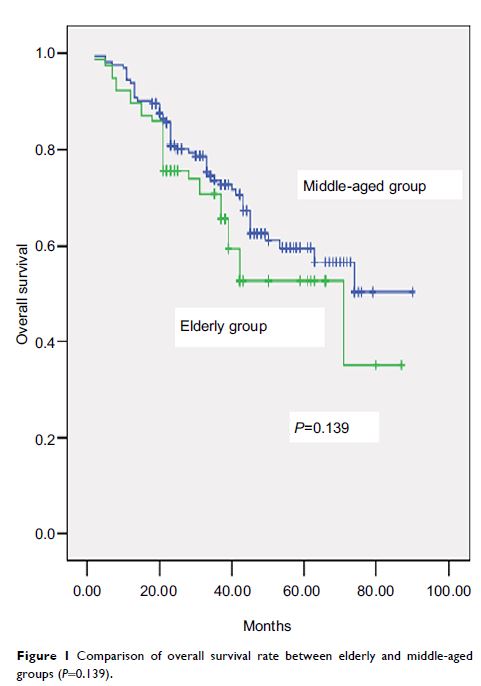
Results: Compared to the middle-aged group, the elderly group had higher
values for Charlson comorbidity index, proportion of preoperative chemotherapy,
and American Society of Anesthesiologists score. No other significant
differences were observed in the preoperative characteristics. The elderly
group had a higher conversion rate, compared to the middle-aged group, although
no significant differences were observed in the surgical procedures, surgical
times, intraoperative blood losses, numbers and severities of postoperative
90-day complications, postoperative 90-day mortality rates, pathology results,
and other short-term outcomes. Long-term follow-up revealed similar rates of
recurrence, disease-free survival, and overall survival in the two groups.
Multivariable analysis revealed that age did not independently predict overall
survival or disease-free survival.
Conclusion: Similar short- and long-term outcomes were observed after LH for
CRLM in elderly and middle-aged patients. Thus, advanced age is not a
contraindication for LH treatment in this setting.
Keywords: laparoscopic hepatectomy, minimally invasive surgery, colorectal
liver metastases, surgical oncology