108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

骨转移预测侵袭性治疗后结直肠癌脑转移患者的预后不良
Authors Duan H, He ZQ, Guo CC, Li JH, Wang J, Zhu Z, Sai K, Chen ZP, Jiang XB, Mou YG
Received 28 March 2018
Accepted for publication 27 May 2018
Published 6 August 2018 Volume 2018:10 Pages 2467—2474
DOI https://doi.org/10.2147/CMAR.S169563
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Cristina Weinberg
Peer reviewer comments 3
Editor who approved publication: Dr Antonella D'Anneo
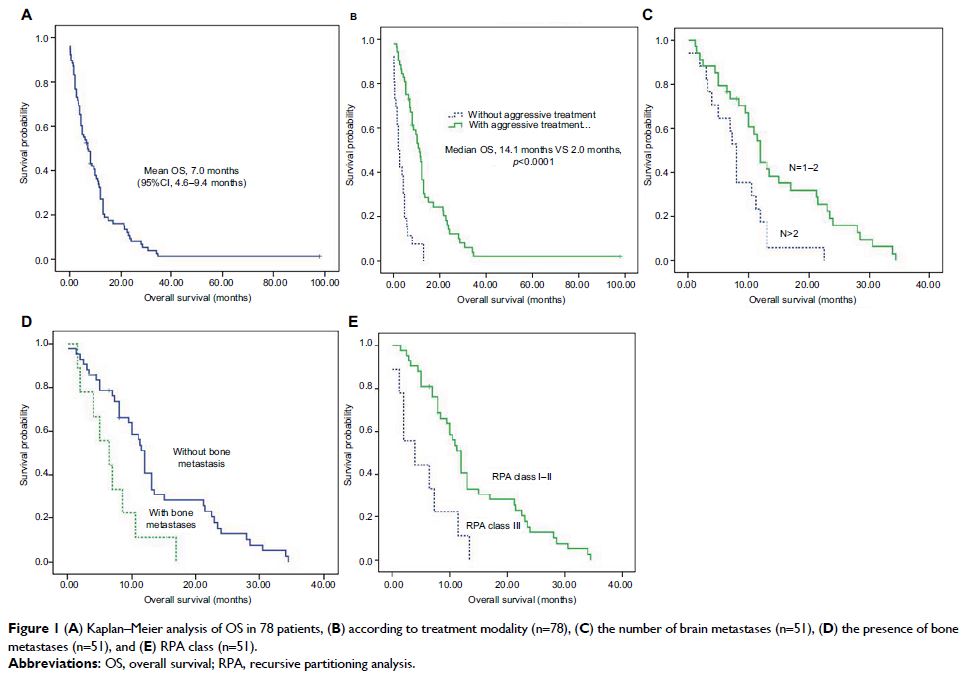
Purpose: The presence of brain metastasis (BM) in patients with colorectal
cancer (CRC) is usually associated with terminal-stage illness; however, a
subgroup of patients receiving aggressive treatment can have a satisfactory
prognosis. This study was designed to investigate the profile of prognostic
factors in CRC patients with BM treated aggressively.
Patients and
methods: CRC patients with BM were
retrospectively reviewed. Survival analysis was performed to identify potential
prognostic factors in the entire cohort of patients and a subgroup of patients
treated aggressively. Aggressive treatments included surgical resection,
radiotherapy, and/or chemotherapy. Overall survival was defined as the time
between the diagnosis of BM and death or until the date of the last follow-up
visit.
Results: A total of 78 CRC patients were confirmed as having BM.
Sixty-eight of them had extracranial metastases at the time of their BM diagnosis.
The most common sites of extracranial metastases were lung (n=51, 65.4%),
followed by liver (n=25, 32.1%) and bone (n=12, 15.4%). Fifty-one patients who
were treated aggressively had significantly longer overall survival than those
who accepted palliative care (14.1 months vs 2.0 months, P <0.0001). Multivariate
analysis was applied, and the results showed that aggressive treatment (n=51),
recursive partitioning analysis class I/II (hazard ratio [HR]=0.27, 95% CI:
0.12–0.6, P =0.001), and fewer BM (HR=0.4,
95% CI: 0.21–0.78, P =0.07) predicted
longer survival. In contrast, the presence of bone metastasis, rather than lung
or liver metastasis, at the time of diagnosis of BM (HR=2.38, 95% CI:
1.08–5.28, P =0.032) predicted a poor
prognosis.
Conclusions: Although the prognosis of CRC patients having BM is frequently
very poor, those with good performance status and few brain lesions responded
to aggressive treatment, while those with bone metastasis at the time of
diagnosis of BM had relatively dismal survival rates, even when treated
aggressively.
Keywords: brain metastasis, colorectal cancer, bone metastasis, aggressive
treatment