108384
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

某些选定的术前炎症评分对接受过根治性前列腺切除术的高风险、局限性前列腺癌患者的预后价值
Authors Shu K, Zheng Y, Chen J, Li W, Jiang K
Received 10 September 2017
Accepted for publication 28 February 2018
Published 3 August 2018 Volume 2018:11 Pages 4551—4558
DOI https://doi.org/10.2147/OTT.S151314
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Cristina Weinberg
Peer reviewer comments 3
Editor who approved publication: Dr Ingrid Espinoza
Background: This study investigated the prognostic value of inflammation-based
scores in patients with high-risk localized prostate cancer who underwent
radical prostatectomy with or without neoadjuvant androgen deprivation therapy
(ADT).
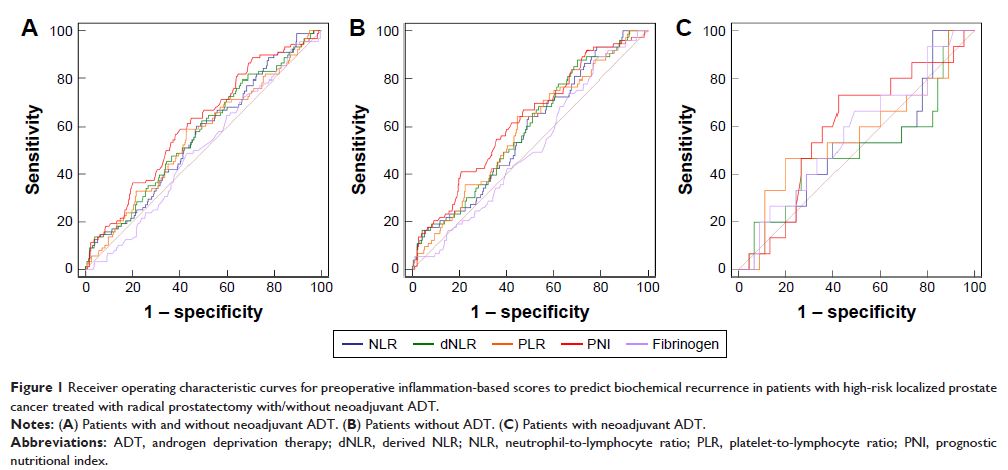
Methods: Inflammation-based scores included the neutrophil-to-lymphocyte
ratio (NLR), derived NLR (dNLR), platelet-to-lymphocyte ratio (PLR), prognostic
nutritional index (PNI), and plasma fibrinogen. A total of 440 patients (380
patients treated without neoadjuvant ADT and 60 patients treated with
neoadjuvant ADT) were retrospectively evaluated in our medical center. Receiver
operating characteristic (ROC) curves and Kaplan–Meier analyses were performed
to compare the prognostic value of these scores. Univariate and multivariate
Cox regression analyses were also performed.
Results: For all patients, dNLR and PNI were predictive of biochemical
recurrence (P =0.041 and <0.001,
respectively). Subgroup analysis of neoadjuvant strategies was also performed.
For patients treated with neoadjuvant ADT, no selected inflammation-based
scores were significantly correlated with biochemical recurrence (P >0.05). In contrast, for
patients treated without neoadjuvant ADT, NLR (area under the ROC curve [AUC]
=0.576, P =0.033), dNLR (P =0.585 and 0.017), PLR (AUC
=0.582,P =0.024), and PNI (AUC =0.622, P <0.001) were predictive
of biochemical recurrence. Kaplan–Meier analyses showed that dNLR (P =0.044), PLR (P =0.028), and PNI (P =0.004) were significantly
associated with biochemical recurrence. Based on multivariable models, PNI was
an independent predictor of biochemical recurrence (hazard ratio: 0.56, 95% confidence
interval: 0.35–0.90, P =0.016).
Conclusion: High dNLR, high PLR, and low PNI were associated with poor
biochemical recurrence-free survival in patients undergoing radical
prostatectomy for high-risk localized prostate cancer not treated with neoadjuvant
ADT. In particular, PNI was an independent prognostic factor for biochemical
recurrence.
Keywords: biochemical recurrence, prostate cancer, derived
neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, prognostic
nutritional index