108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

原发肿瘤手术治疗小涎腺腺癌远处转移的预后价值:来自基于 SEER 的研究的第一个证据
Authors Shi X, Huang NS, Shi RL, Wei WJ, Wang YL, Ji QH
Received 2 May 2018
Accepted for publication 5 June 2018
Published 20 July 2018 Volume 2018:10 Pages 2163—2172
DOI https://doi.org/10.2147/CMAR.S172725
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Andrew Yee
Peer reviewer comments 2
Editor who approved publication: Professor Nakshatri
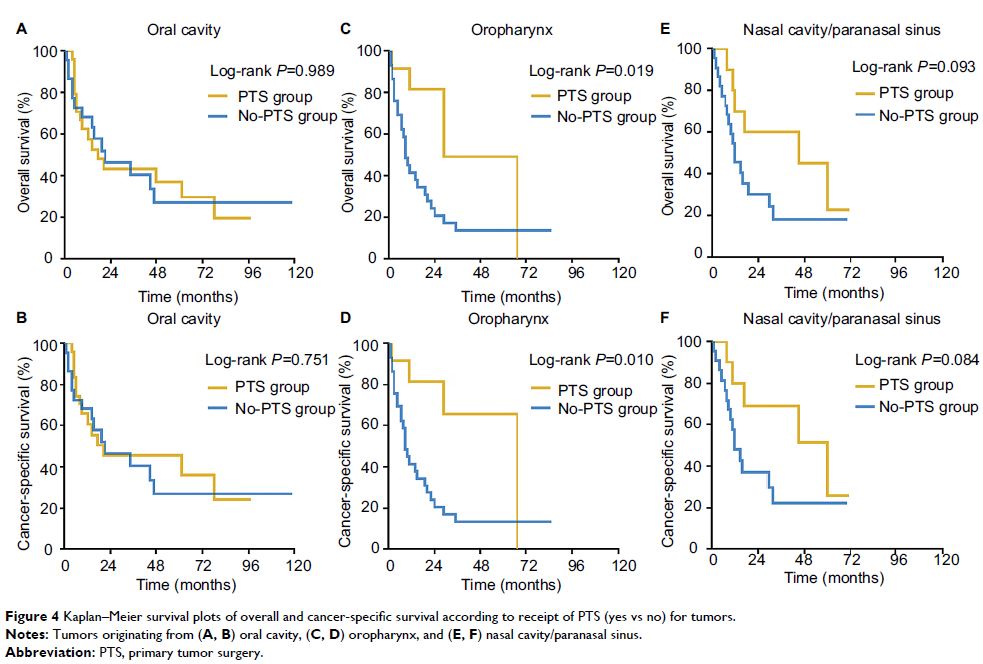
Purpose: The prognostic value of primary tumor surgery (PTS) in minor
salivary-gland carcinoma (MiSGC) with distant metastasis (DM) at diagnosis has
never been investigated. In this study, we aimed to provide the first evidence.
Patients and
methods: The Surveillance, Epidemiology, and
End Results (SEER) database was employed to identify MiSGC patients with DM at
diagnosis. The prognostic value of PTS was evaluated by Kaplan–Meier methods,
log-rank analyses, and multivariate Cox proportional-hazard regression models.
Results: Of the 152 eligible patients included in our study, 50 (32.9%) had
undergone PTS. Kaplan–Meier analyses showed that the PTS group had >20%
increase in 1- and 2-year overall survival (OS) and cancer-specific survival
(CSS) compared with their counterparts without PTS (PTS group vs no-PTS group,
1-year OS 66.1% vs 43.9%, 1-year CSS 69.9% vs 44.9%, 2-year OS 56.6% vs 24.2%,
2-year CSS 59.9% vs 25.7%). Compared with the no-PTS group, multivariate
analyses also demonstrated a significantly decreased risk of overall mortality
(HR 0.601, 95% CI 0.379–0.952; P =0.031) and
cancer-specific mortality (HR 0.547, 95% CI 0.336–0.891; P =0.015) in the PTS group.
Subgroup multivariate analyses revealed patients with T1–T3 oropharynx, nasal
cavity, or paranasal sinus primary MiSGC, especially adenoid cystic carcinoma,
might benefit from PTS (all P <0.05).
Conclusion: PTS is associated with improved survival in highly selected MiSGC
patients and may be considered in future clinical practice. However,
prospective studies with larger sample size are still necessary to validate our
findings.
Keywords: minor salivary gland carcinoma, distant metastasis, primary tumor
surgery, T stage, primary site, SEER