108384
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

颈椎矢状位对准作为邻近骨化发育的预测因子
Authors Liu W, Rong Y, Chen J, Luo Y, Tang P, Zhou Z, Fan J, Cai W
Received 21 December 2017
Accepted for publication 6 June 2018
Published 20 July 2018 Volume 2018:11 Pages 1359—1366
DOI https://doi.org/10.2147/JPR.S160472
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Andrew Yee
Peer reviewer comments 3
Editor who approved publication: Dr Erica Wegrzyn
Purpose: To explore the role of cervical sagittal alignment in the
occurrence of adjacent-level ossification development (ALOD) in patients who
underwent anterior cervical discectomy fusion with self-locking stand-alone
polyetheretherketone cage, and the relationship between cervical sagittal
alignment and clinical outcomes.
Background: Because of its advantages, anterior cervical
plating systems have been used as the classic surgical method in the treatment
of patients with cervical disc herniation. However, the proximity (<5 mm) of
the plate to the adjacent disc space has proven to be a critical risk factor
for ALOD. How cervical sagittal alignment influences the development of ALOD is
unknown and its role in ALOD needs clarification.
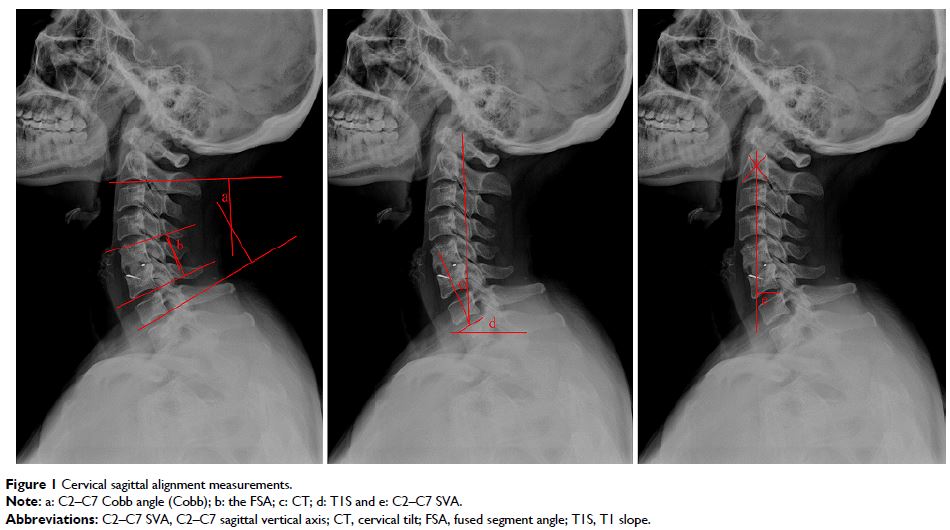
Patients and methods: One hundred and eighteen adults who underwent
anterior cervical discectomy fusion with self-locking stand-alone
polyetheretherketone cage for cervical radiculopathy or myelopathy between
December 2013 and December 2015 were retrospectively recruited. Of these, 15
patients developed ALOD and 103 patients did not, representing two groups for
comparison. The cervical sagittal parameters were measured, including C2–C7
Cobb angle (Cobb), fused segment angle, cervical tilt (CT), T1 slope (T1S) and
C2–C7 sagittal vertical axis. Clinical outcomes and efficacy were evaluated
using a visual analog scale, Japanese Orthopedic Association (JOA) score and
neck disability index (NDI) score before and after surgery.
Results: There were no significant differences in patient
demographics between the two groups. Cobb value (P <0.05),
CT (P <0.05) and T1S (P <0.05) were significantly
different between the two groups, while fused segment angle (P >0.05) and C2–C7 sagittal
vertical axis (P >0.05) showed no difference.
Compared with preoperative scores, improvement was seen in postoperative visual
analog scale, JOA and NDI scores at each time point (P <0.05). However, the
postoperative scores at 24 months in the NO-ALOD group indicated greater
improvements compared with the ALOD group (P <0.05). There
were significant correlations between Cobb and CT (r =0.607, P <0.05) and CT and T1S (r =0.681, P <0.05). Also, T1S was
significantly correlated with clinical outcomes (JOA: r =0.689, P <0.05; NDI: r =−0.710, P <0.05).
Conclusion: Maintaining a lordotic cervical sagittal
alignment was related to a lower risk of ALOD and improved clinical outcomes.
Keywords: adjacent-level
ossification development, cervical sagittal alignment, clinical outcomes,
stand-alone anchored cage