108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

关于新辅助化放疗加抗 EGFR 单克隆抗体,随后进行局部晚期宫颈癌手术的一项前瞻性研究
Authors Lu H, Wu Y, Liu X, Jiang H, Pang Q, Peng L, Cheng J, Deng S, Gu J, Zhao R, Hu X, Chen C, Yu J
Received 29 January 2018
Accepted for publication 10 May 2018
Published 2 July 2018 Volume 2018:11 Pages 3785—3792
DOI https://doi.org/10.2147/OTT.S164071
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Lucy Goodman
Peer reviewer comments 2
Editor who approved publication: Dr Jianmin Xu
Background: To investigate the efficacy and safety of neoadjuvant
chemoradiotherapy plus anti-epidermal growth factor receptor monoclonal
antibody followed by surgery for locally advanced cervical cancer (LACC).
Patients and methods: Patients with histologically proven LACC were
enrolled into this prospective study. All patients received intensity-modulated
radiation therapy with conventional fractionation. Weekly cisplatin or
nedaplatin was administered concurrently with intensity-modulated radiation
therapy. Nimotuzumab, a humanized anti-epidermal growth factor receptor
monoclonal antibody, was given at a dose of 200 mg per week for 6 cycles.
Approximately 1 month after the completion of neoadjuvant treatment, the
patients were assessed for clinical tumor response and operability based on MRI
and gynecological examination. For those who were considered to be candidates
for surgery, radical hysterectomy, and pelvic lymph node dissection were
performed 5–6 weeks after the completion of neoadjuvant therapy.
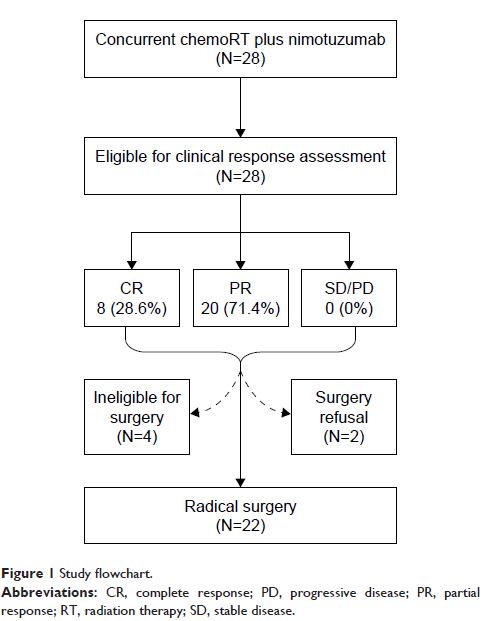
Results: Twenty-eight patients were enrolled. Clinical
complete response and partial response were found in 8 (28.5%) and 20 (71.5%)
patients, respectively. Four patients were not eligible for surgery and 2
patients refused surgery although they were assessed as surgical candidates.
They were not included in this analysis. Radical hysterectomy and pelvic lymph
node dissection were performed for the remaining 22 patients. Among them, 8
(36.4%) had complete pathology response, 9 (40.9%) presented with persistent
atypical cells or cervical intraepithelial neoplasia, and 5 (22.7%) presented
with macroscopic and/or microscopic residual disease, according to the
pathological evaluation. Median follow-up time was 22 months (range, 5–39
months). The 2-year locoregional control rate, progression-free survival rate,
distant metastasis-free survival rate, and overall survival rate were 95.0%,
85.2%, 84.0%, and 90.0%, respectively. Acute toxicities were mild in general
and easily manageable. Chronic toxicities were mainly limited to grade 1. No
severe late toxicities were observed.
Conclusion: Concurrent chemoradiotherapy plus nimotuzumab
followed by surgery is highly effective and safe in LACC. Further studies are
warranted to confirm the findings.
Keywords: locally
advanced cervical cancer, neoadjuvant chemotherapy, intensity-modulated
radiotherapy, anti-EGFR monoclonal antibody, radical surgery, hysterectomy