108384
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

接受贝伐单抗联合治疗的新确诊的胶质母细胞瘤患者的预后:一项综合分析
Authors Liao KL, Huang S, Wu YP
Received 10 November 2017
Accepted for publication 20 February 2018
Published 19 June 2018 Volume 2018:11 Pages 3513—3520
DOI https://doi.org/10.2147/OTT.S156723
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Justinn Cochran
Peer reviewer comments 5
Editor who approved publication: Dr Yao Dai
Background: A combination of temozolomide (TMZ) and radiotherapy and
subsequent adjuvant chemotherapy is the gold standard of treatment for
glioblastoma (GB). Bevacizumab (BEV), a humanized monoclonal antibody that
blocks the effects of vascular endothelial growth factor A, has produced
impressive response rates for recurrent GB and has been approved as second-line
therapy. The efficacy and safety of BEV in newly diagnosed GB are not known.
Aim: This systematic meta-analysis was undertaken to evaluate the value
of combination therapy involving BEV in newly diagnosed GB.
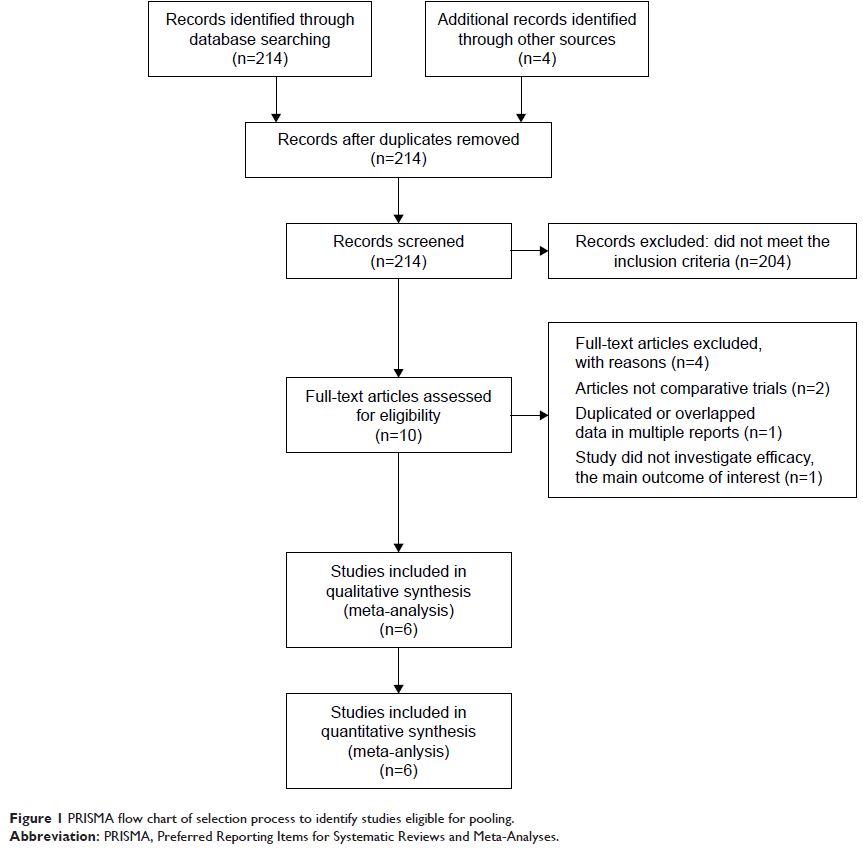
Methods: Electronic databases were searched for eligible literature up to
October 2017. Randomized controlled trials assessing the efficacy and safety of
BEV in patients with newly diagnosed GB were included, of which the main
outcomes were progression-free survival (PFS), overall survival (OS), and
adverse events (AEs). All the data were pooled with the corresponding 95%
confidence intervals (CIs) using RevMan software. Sensitivity analyses and
heterogeneity were quantitatively evaluated.
Results: A total of six randomized controlled trials were included in this
analysis. The experimental BEV group had significantly improved the overall PFS
(OR =0.46, 95% CI =0.26–0.81, P =0.007), as well
as PFS at 6 months (OR =3.47, 95% CI =2.85–4.22, P <0.00001) and PFS at
12 months (OR =2.02, 95% CI =1.66–2.46, P <0.00001),
respectively. However, there were no significant differences in PFS at
24 months with BEV (OR =0.95, 95% CI =0.61–1.48, P =0.82). OS at 6 months (P =0.07) and 24 months (P =0.07) was not significantly
improved with BEV in patients with newly diagnosed GB. However, the
meta-analysis on the OS at 12 months showed differences with BEV (OR
=1.24, 95% CI =1.03–1.50, P =0.02).
Conclusion: Our study indicates that addition of BEV for newly diagnosed GB
resulted in a superior PFS rate. However, the combination therapy involving BEV
did not improve OS. Future investigations are needed to analyze whether BEV
helps improve OS efficacy.
Keywords: bevacizumab, glioblastoma, newly diagnosed, meta-analysis,
neoadjuvant