108384
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

已发表论文
姑息性放疗在不能切除的肝内胆管细胞癌中的作用:基于人口的分析与倾向评分匹配
Authors Shao F, Qi W, Meng FT, Qiu L, Huang Q
Received 23 December 2017
Accepted for publication 13 April 2018
Published 13 June 2018 Volume 2018:10 Pages 1497—1506
DOI https://doi.org/10.2147/CMAR.S160680
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Cristina Weinberg
Peer reviewer comments 4
Editor who approved publication: Professor Luzhe Sun
Background: This
population-based study evaluated the overall (OS) and cancer-specific survival
(CSS) benefit from palliative radiotherapy (RT) in patients with unresectable
intrahepatic cholangiocarcinoma (ICC).
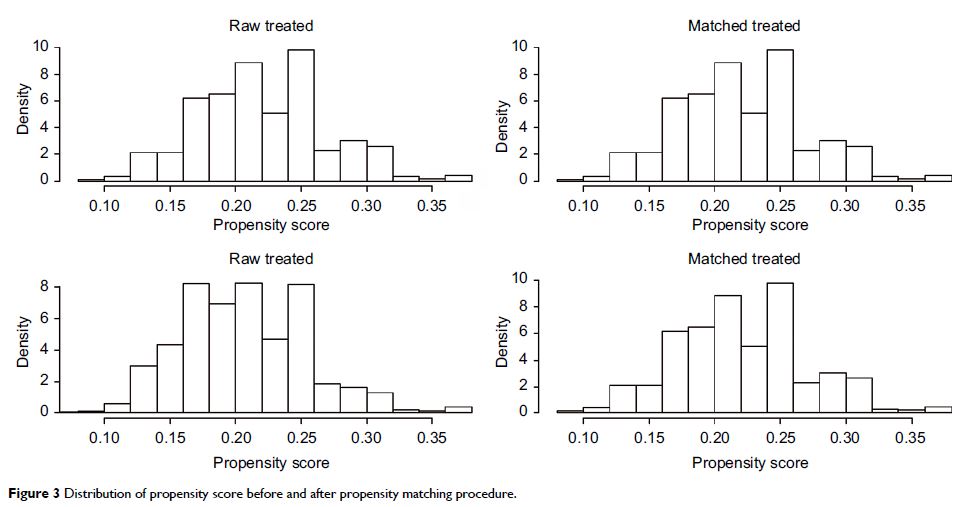
Methods: We queried The Surveillance, Epidemiology, and End Results (SEER) database for the patients with unresectable ICC diagnosed from 1973 to 2013. Propensity score–matched analysis was performed to reduce the impact of the selection bias between the palliative RT group and the nonpalliative RT group. Kaplan–Meier survival curves were used to estimate the survival outcome before and after propensity score matching. OS and CSS were compared between patients with and without palliative RT using univariate and multivariate Cox proportional hazards regression analyses.
Results: A total of 4,027 of 15,803 patients diagnosed with ICC were included in this study. Of those, 847 (21%) patients underwent palliative RT, whereas 3,180 (79%) did not. In the unmatched population, patients treated with palliative RT had improved OS and CSS relative to those treated without palliative RT (adjusted HR =0.9065, 95% CI =0.8360–0.982, P =0.01735) and CSS (adjusted HR =0.8874, 95% CI =0.8160–0.9652, P =0.00532). After propensity score matching, palliative RT was associated with a significantly improved OS (adjusted HR =0.8544, 95% CI =0.7722–0.9453, P =0.00228) and CSS (adjusted HR =0.8563, 95% CI =0.7711–0.9509, P =0.0037).
Conclusion: Palliative RT seems to improve the prognosis of patients with unresectable ICC.
Keywords: radiation therapy, SEER, unresectable intrahepatic cholangiocarcinoma
Methods: We queried The Surveillance, Epidemiology, and End Results (SEER) database for the patients with unresectable ICC diagnosed from 1973 to 2013. Propensity score–matched analysis was performed to reduce the impact of the selection bias between the palliative RT group and the nonpalliative RT group. Kaplan–Meier survival curves were used to estimate the survival outcome before and after propensity score matching. OS and CSS were compared between patients with and without palliative RT using univariate and multivariate Cox proportional hazards regression analyses.
Results: A total of 4,027 of 15,803 patients diagnosed with ICC were included in this study. Of those, 847 (21%) patients underwent palliative RT, whereas 3,180 (79%) did not. In the unmatched population, patients treated with palliative RT had improved OS and CSS relative to those treated without palliative RT (adjusted HR =0.9065, 95% CI =0.8360–0.982, P =0.01735) and CSS (adjusted HR =0.8874, 95% CI =0.8160–0.9652, P =0.00532). After propensity score matching, palliative RT was associated with a significantly improved OS (adjusted HR =0.8544, 95% CI =0.7722–0.9453, P =0.00228) and CSS (adjusted HR =0.8563, 95% CI =0.7711–0.9509, P =0.0037).
Conclusion: Palliative RT seems to improve the prognosis of patients with unresectable ICC.
Keywords: radiation therapy, SEER, unresectable intrahepatic cholangiocarcinoma