108899
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

高敏心肌肌钙蛋白 T 与非急性冠脉综合征老年住院患者预后的关系
Authors Wu W, Li DX, Wang Q, Xu Y, Cui YJ
Received 14 November 2017
Accepted for publication 5 March 2018
Published 6 June 2018 Volume 2018:13 Pages 1091—1098
DOI https://doi.org/10.2147/CIA.S157048
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Dr Wu
Objective: Low-level high-sensitivity cardiac troponin T (hs-cTnT) increases
in elderly population. In this study, the relationship between hs-cTnT level
and all-cause death of elderly inpatients with non-acute coronary syndrome
(non-ACS) after discharge from the hospital was investigated.
Materials and
methods: Non-ACS patients aged >65 years
admitted in the General Practice Wards and Department of Geriatrics of Fuxing
Hospital Affiliated to Capital Medical University were enrolled in the study.
The patients were grouped according to the tertiles of hs-cTnT levels.
Biochemical markers, hs-cTnT, and amino-terminal pro-brain natriuretic peptide
were measured. The median follow-up period was 47 months, and all-cause deaths
of the patients were observed.
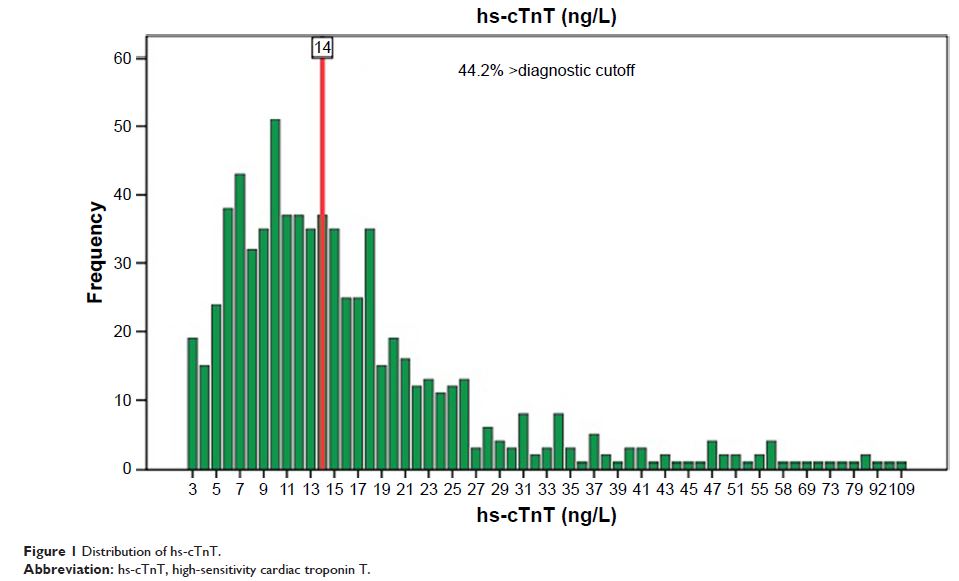
Results: A total of 722 patients, including 473 males and 249 females, aged
65–98 (82.43±5.98) years were enrolled in the study. The level of hs-cTnT was
found to be higher in males, and increased with age and comorbidities (P <0.01). Compared with low-level
group, NT-proBNP level of patients in high-level group was higher, while
hemoglobin (Hb), estimated glomerular filtration rate (eGFR), and left
ventricular ejection fraction (LVEF) levels were lower (P <0.001). The mortality rate
increased significantly with increased hs-cTnT levels (P <0.001). The total number of
deaths was 136 (18.8%), and of these, 108 (79.4%) were noncardiac deaths. Risk
of all-cause deaths in the highest hs-cTnT level group was 7.3 times higher
than that of the lowest hs-cTnT level group (95% CI: 4.29–12.51, P <0.001). After adjusting for
gender, age, comorbidities, NT-proBNP, Hb, eGFR, and LVEF, hs-cTnT level still
affected the patient’s survival time (HR: 3.01, 95% CI: 1.67–5.43, P <0.001).
Conclusion: These findings suggest that low-level hs-cTnT was increased in
elderly inpatients without ACS. They further highlight that baseline hs-cTnT
level was associated with increased risk of all-cause deaths among patients
after their discharge, and most deaths were from non-cardiovascular diseases.
Keywords: high-sensitivity cardiac troponin T, elderly inpatients, non-acute
coronary syndrome, prognosis