108384
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

经卡非佐米治疗的复发和难治性多发性骨髓瘤患者的心脏毒性发生率和风险
Authors Zhao F, Yang B, Wang J, Zhang R, Liu J, Yin F, Xu W, He C
Received 14 December 2017
Accepted for publication 12 January 2018
Published 30 May 2018 Volume 2018:12 Pages 1525—1531
DOI https://doi.org/10.2147/DDDT.S159818
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Palas Chanda
Peer reviewer comments 2
Editor who approved publication: Dr Anastasios Lymperopoulos
Purpose: Carfilzomib has been approved for use in relapsed and refractory
multiple myeloma (RRMM). Cardiac toxicities have been reported with the use of
carfilzomib. We aimed to determine the overall incidence and risk of cardiac
toxicities in RRMM patients treated with carfilzomib using a meta-analysis.
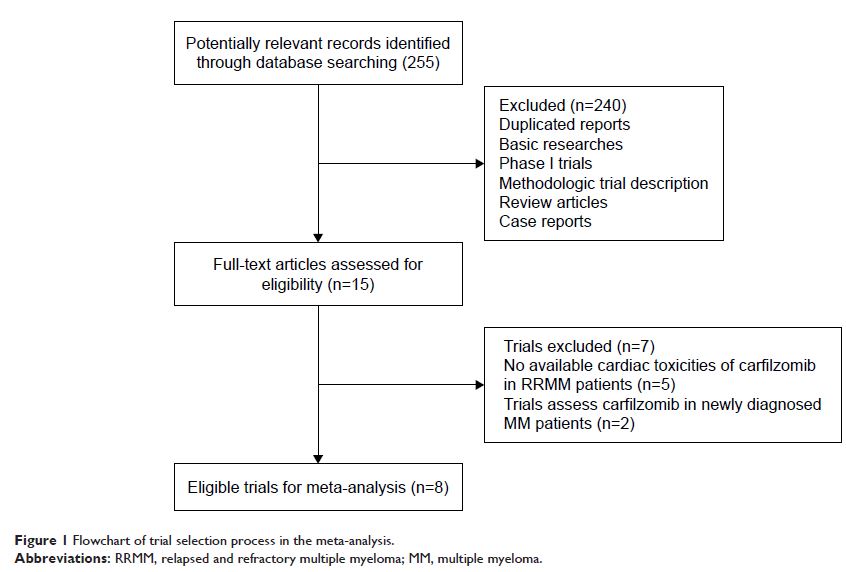
Methods: We searched several databases for relevant articles. Prospective
trials evaluating carfilzomib in RRMM patients with adequate data on cardiac
toxicities were included for analysis. Pooled incidence, Peto ORs, and 95% CIs were
calculated according to the heterogeneity of selected studies.
Results: A total of 2,607 RRMM patients from eight prospective trials were
included. The pooled incidence of all-grade congestive heart failure (CHF) and
ischemic heart disease (IHD) related to carfilzomib in RRMM patients was 5.5%
(95% CI: 4.3%–6.9%) and 2.7% (95% CI: 1.1%–6.7%), respectively. In addition,
the use of carfilzomib significantly increased all-grade (Peto OR 2.33, 95% CI:
1.56–3.48, p <0.001) and high-grade (Peto
OR 3.22, 95% CI: 1.84–5.61, p <0.001) CHF
when compared to controls, whereas there was no significantly increased risk of
developing all-grade (Peto OR 1.31, 95% CI: 0.79–2.18, p =0.30) and high-grade (Peto OR
1.41, 95% CI: 0.73–2.72, p =0.31) IHD in RRMM
patients receiving carfilzomib.
Conclusion: The use of carfilzomib in RRMM patients significantly increases
the risk of developing CHF but not IHD. Clinicians should be cautious about the
risk of CHF associated with carfilzomib to maximize the benefits and minimize
the toxicities.
Keywords: carfilzomib, cardiac toxicities, clinical trials, meta-analysis,
congestive heart failure, ischemic heart disease