109669
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

用于预测前哨淋巴结阳性乳腺癌患者的非前哨淋巴结转移的纪念斯隆·凯特琳癌症中心列线图的验证
Authors Bi X, Wang Y, Li M, Chen P, Zhou Z, Liu Y, Zhao T, Zhang Z, Wang C, Sun X, Qiu P
Published Date February 2015 Volume 2015:8 Pages 487—493
DOI http://dx.doi.org/10.2147/OTT.S78903
Received 8 December 2014, Accepted 8 January 2015, Published 23 February 2015
Background: The main
purpose of the study reported here was to validate the clinical value of the
Memorial Sloan Kettering Cancer Center (MSKCC) nomogram that predicts
non-sentinel lymph node (SLN) metastasis in SLN-positive patients with breast
cancer.
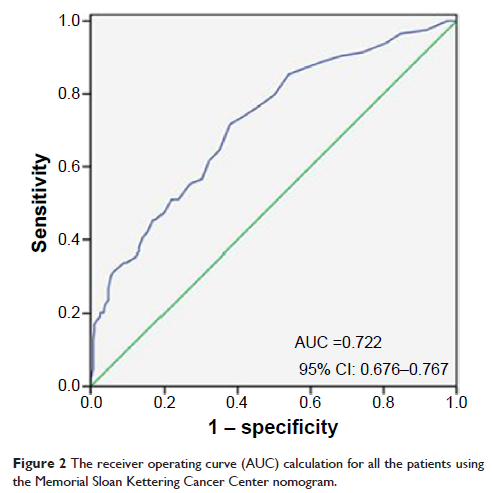
Methods: Data on 1,576 patients
who received sentinel lymph node biopsy (SLNB) at the Shandong Cancer Hospital
from December 2001 to March 2014 were collected in this study, and data on 509
patients with positive SLN were analyzed to evaluate the risk factors for non-SLN
metastasis. The MSKCC nomogram was used to estimate the probability of non-SLN
metastasis and was compared with actual probability after grouping into
deciles. A receiver-operating characteristic (ROC) curve was drawn and
predictive accuracy was assessed by calculating the area under the ROC curve.
Results: Tumor size,
histological grade, lymphovascular invasion, multifocality, number of positive
SLNs, and number of negative SLNs were correlated with non-SLN metastasis (P <0.05) by univariate analysis.
However, multivariate analysis showed that tumor size (P =0.039), histological grade (P =0.043), lymphovascular invasion (P =0.001), number of positive SLNs (P =0.001), and number of negative
SLNs (P =0.000) were identified as
independent predictors for non-SLN metastasis. The trend of actual probability
in various decile groups was comparable to the predicted probability. The area
under the ROC curve was 0.722. Patients with predictive values lower than 10%
(97/492, 19.7%) had a frequency of non-SLN metastasis of 17.5% (17/97).
Conclusion: The MSKCC nomogram
can provide an accurate prediction of the probability of non-SLN metastasis,
and offers a reference basis about axillary lymph node dissection. Axillary
lymph node dissection could be avoided in patients with predictive values lower
than 10%.
Keywords: MSKCC nomogram,
probability, SLN, axillary lymph node dissection, risk factors