108985
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

利用睑板腺内注射抗 VEGF 剂贝伐单抗治疗睑板腺血管挛缩引起的睑板腺功能障碍的功效
Authors Jiang X, Wang Y, Lv H, Liu Y, Zhang M, Li X
Received 16 July 2017
Accepted for publication 23 March 2018
Published 16 May 2018 Volume 2018:12 Pages 1269—1279
DOI https://doi.org/10.2147/DDDT.S146556
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Amy Norman
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Frank Boeckler
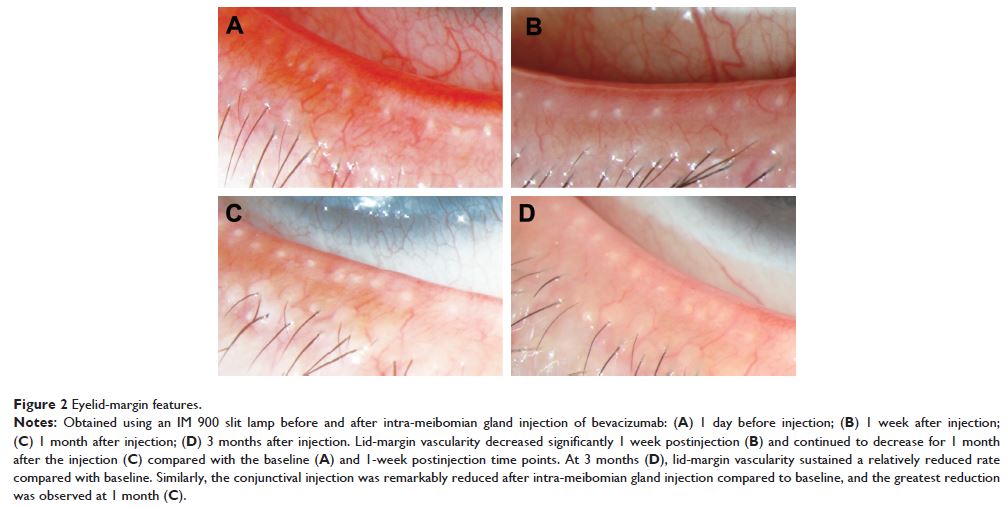
Purpose: To investigate the efficacy of a novel treatment – intra-meibomian
gland (MG) injection of the anti-VEGF agent bevacizumab – for MG dysfunction
(MGD) with eyelid-margin vascularity.
Methods: A total of 26 eyes from 13 patients diagnosed with MGD and
eyelid-margin vascularity were included in our study. Patients received
intra-meibomian gland injections of bevacizumab (150 µL, 2.5 mg/0.1 mL) at
multiple sites with a 29 G needle where telangiectasia was severe. The Ocular
Surface Disease Index (OSDI), tear film, tear-breakup time (TBUT),
eyelid-margin features, MG features, conjunctiva, and corneal staining were
assessed at 1 day before injection and 1 week, 1 month, and 3 months after
injection. Blood pressure, best-corrected visual acuity, intraocular pressure,
and slit lamp examinations were performed to assure the safety of patients at 1
day before and 1 day, 1 week, 1 month, and 3 months after injection.
Results: Lid-margin vascularity, conjunctival injection, expressed
secretion quality, expressivity of the MG, TBUT, corneal staining, and OSDI
were significantly improved 1 week, 1 month, and 3 months after injection
compared to baseline values. Lid-margin vascularity, conjunctival injection,
meibomian gland expressivity, TBUT, and OSDI continued to improve; the greatest
improvements were observed at 1 month and sustained for 3 months. Spearman’s
correlation analysis indicated that age and sex significantly influenced TBUT
improvement. Females and older patients tended to have shorter baseline TBUT
that followed a different trend from that of males and younger patients during
postinjection visits, revealed by subgroup analysis. No local or systemic side
effects were observed at follow-up visits.
Conclusion: This study is the first to explore a novel therapy for MGD –
intra-MG injection of the anti-VEGF agent bevacizumab – and it demonstrates
that the treatment is effective and safe in eliminating eyelid-margin
vascularity, improving MG function and relieving clinical signs and symptoms of
MGD.
Keywords: meibomian gland dysfunction, anti-VEGF, lid-margin vascularity