108985
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

大块非小细胞肺癌的部分立体定向消融放疗: 一项回顾性研究
Authors Bai Y, Gao XS, Qin SB, Chen JY, Su MM, Liu Q, Qin XB, Ma MW, Zhao B, Gu XB, Xie M, Cui M, Qi X, Li XY
Received 11 December 2017
Accepted for publication 27 March 2018
Published 8 May 2018 Volume 2018:11 Pages 2571—2579
DOI https://doi.org/10.2147/OTT.S159538
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Manfred Beleut
Peer reviewer comments 2
Editor who approved publication: Dr Yao Dai
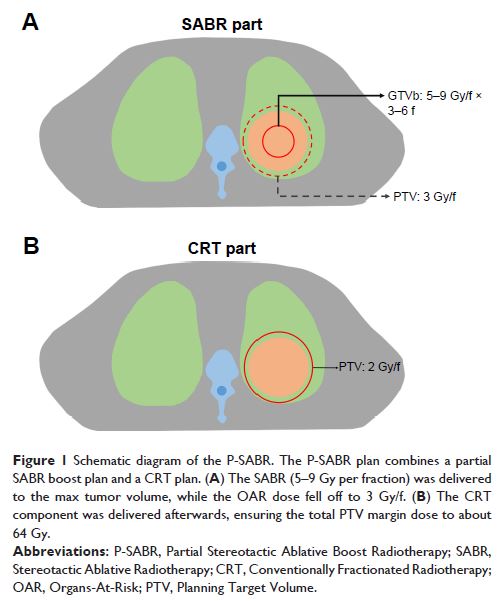
Purpose: Bulky non-small cell lung cancer (NSCLC) is difficult to achieve
effective local control by conventionally fractionated radiotherapy (CRT). The
present work aims to evaluate the safety and efficacy of partial stereotactic
ablative boost radiotherapy (P-SABR) in bulky NSCLC.
Patients and
methods: From December 2012 through August
2017, 30 patients with bulky NSCLC treated with P-SABR technique were analyzed.
The P-SABR plan consisted of one partial SABR plan (5–9 Gy/f, 3–6 fractions) to
gross tumor boost (GTVb), followed by one CRT plan to the planning target
volume (PTV). GTVb was the max volume receiving SABR to guarantee the dose of organs-at-risks
(OARs) falloff to about 3 Gy/f. The total dose of PTV margin was planned to
above 60 Gy. The simply CRT plans were created using the same planning
parameters as the original plan, with the goal to achieve comparable OARs doses
and PTV margin dose to the P-SABR plan. Dosimetric variables were acquired in
both P-SABR and compared CRT plans. Toxicity, local control, and survival were
also evaluated.
Results: Median follow-up in survivors was 10.3 months (range=2.3–39.4
months). Eleven patients (36.7%) had partial response (PR) and ten patients
(33.3%) had stable disease (SD). Two-year overall survival was 55.6%. Two-year
local control rate was 85.7%. No severe acute side effects. CTCAE Grade III
were observed. Compared to the simply CRT plan, P-SABR plans achieved similar
doses to the OARs and Dmin, but increased dose at the isocenter, Dmean, Dmax,
and biological equivalent dose (BED) significantly (P<0.05).
BED in the tumor center could reach 107.3 Gy (93.2–132 Gy). Patients with
B90≥65% achieved a higher local control rate than those with B90<65% (P =0.010).
Conclusion: This retrospective study suggests that P-SABR is feasible and well
tolerated in bulky NSCLC. Local control rate is encouraging, especially for the
B90≥65% group, which may due to the ability of P-SABR to optimize BED with
equivalent toxicity.
Keywords: P-SABR, radiotherapy, NSCLC, bulky mass