108985
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

已发表论文
曲美他嗪对有心肌梗死和抑郁症大鼠的 血清素表达和血清素转移的有益效果
Authors Liu MY, Wei WL, Stone CR, Zhang LJ, Tian GX, Ding JN
Received 18 November 2017
Accepted for publication 5 February 2018
Published 16 March 2018 Volume 2018:14 Pages 787—797
DOI https://doi.org/10.2147/NDT.S157441
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Prof. Dr. Roumen Kirov
Peer reviewer comments 2
Editor who approved publication: Professor Wai Kwong Tang
Background: Trimetazidine is an
anti-ischemic drug that can inhibit platelet aggregation and regulate serotonin
(5-hydroxytryptamine [5-HT]) release. The purpose of this study was to
investigate the therapeutic effects of trimetazidine on 5-HT and serotonin
transporter (SERT) expression in experimentally induced myocardial infarction
(MI), depression, and MI + depression.
Materials and methods: Eighty Sprague Dawley (SD) rats were randomly divided into a trimetazidine group and a saline group of 40 rats each. The trimetazidine group was given trimetazidine pretreatment for 4 weeks, while the saline group received saline for 4 weeks. Both groups were then subdivided into four subgroups (n=10), which were each subjected to a unique disease condition: sham surgery, MI, depression, or MI + depression. All rats were sacrificed 3 days thereafter, and serum and platelet levels of 5-HT and SERT were assessed. In addition, we experimented with trimetazidine posttreatment. Twenty SD rats underwent MI surgery, and were then randomly divided into a treatment and a saline group (n=10 each). For 4 weeks post-surgery, the trimetazidine group was given trimetazidine, while the saline group received saline. Serum and platelet levels of 5-HT and SERT were assessed.
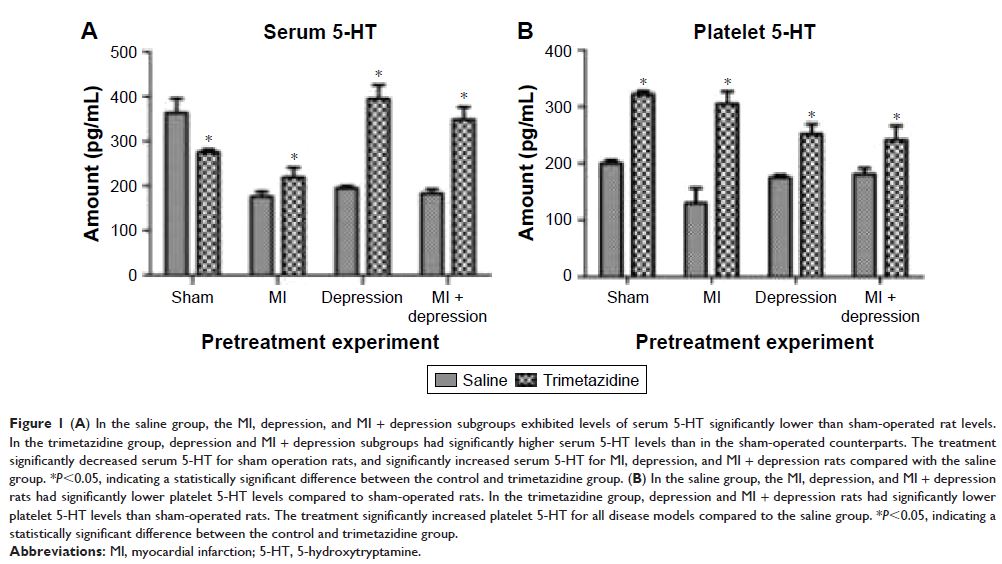
Results: Pretreatment with trimetazidine: in the nontreatment saline group, MI, depression, and MI + depression showed significant declines (P <0.05) in both serum and platelet 5-HT levels compared to sham. Trimetazidine treatment significantly increased serum and platelet 5-HT levels in the MI, depression, and MI + depression (P <0.05) subgroups compared to their counterparts in the saline group. Results for SERT were heterogeneous between serum and platelets. Trimetazidine treatment significantly decreased serum levels of SERT in the sham surgery subgroup (P <0.05), while significantly increasing levels in depression rats, compared to control (P <0.05). In platelets, trimetazidine significantly decreased SERT in sham surgery, MI, depression, and MI + depression rats, compared to control (P <0.05). This contrast suggests that trimetazidine has opposite effects in serum and platelet SERT levels for the three disease models. Post-surgery trimetazidine: increased serum 5-HT (P <0.05) and serum SERT (P <0.05) were observed, compared to control. In platelets, trimetazidine decreased both 5-HT and SERT compared to control, significantly (P <0.05) for 5-HT, but not significantly for SERT (P >0.05).
Conclusion: Trimetazidine has a regulatory effect on 5-HT and SERT in the serum and platelets. Because of the downstream effects of this regulation on blood vessel function and myocardial protection, trimetazidine may be a therapeutic or preventive agent in several disease processes, including MI, depression, and the comorbidity between these two diseases. Further investigation, aimed at exploring the clinical potential of trimetazidine, is therefore warranted.
Keywords: trimetazidine, MI, depression, serotonin, serotonin transporter
Materials and methods: Eighty Sprague Dawley (SD) rats were randomly divided into a trimetazidine group and a saline group of 40 rats each. The trimetazidine group was given trimetazidine pretreatment for 4 weeks, while the saline group received saline for 4 weeks. Both groups were then subdivided into four subgroups (n=10), which were each subjected to a unique disease condition: sham surgery, MI, depression, or MI + depression. All rats were sacrificed 3 days thereafter, and serum and platelet levels of 5-HT and SERT were assessed. In addition, we experimented with trimetazidine posttreatment. Twenty SD rats underwent MI surgery, and were then randomly divided into a treatment and a saline group (n=10 each). For 4 weeks post-surgery, the trimetazidine group was given trimetazidine, while the saline group received saline. Serum and platelet levels of 5-HT and SERT were assessed.
Results: Pretreatment with trimetazidine: in the nontreatment saline group, MI, depression, and MI + depression showed significant declines (P <0.05) in both serum and platelet 5-HT levels compared to sham. Trimetazidine treatment significantly increased serum and platelet 5-HT levels in the MI, depression, and MI + depression (P <0.05) subgroups compared to their counterparts in the saline group. Results for SERT were heterogeneous between serum and platelets. Trimetazidine treatment significantly decreased serum levels of SERT in the sham surgery subgroup (P <0.05), while significantly increasing levels in depression rats, compared to control (P <0.05). In platelets, trimetazidine significantly decreased SERT in sham surgery, MI, depression, and MI + depression rats, compared to control (P <0.05). This contrast suggests that trimetazidine has opposite effects in serum and platelet SERT levels for the three disease models. Post-surgery trimetazidine: increased serum 5-HT (P <0.05) and serum SERT (P <0.05) were observed, compared to control. In platelets, trimetazidine decreased both 5-HT and SERT compared to control, significantly (P <0.05) for 5-HT, but not significantly for SERT (P >0.05).
Conclusion: Trimetazidine has a regulatory effect on 5-HT and SERT in the serum and platelets. Because of the downstream effects of this regulation on blood vessel function and myocardial protection, trimetazidine may be a therapeutic or preventive agent in several disease processes, including MI, depression, and the comorbidity between these two diseases. Further investigation, aimed at exploring the clinical potential of trimetazidine, is therefore warranted.
Keywords: trimetazidine, MI, depression, serotonin, serotonin transporter