108985
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

接受新辅助化疗治疗的乳腺癌患者的外周炎症/化疗敏感性免疫指标及预后
Authors Qian Y, Tao J, Li X, Chen H, Lu Q, Yang J, Pan H, Wang C, Zhou W, Liu X
Received 7 August 2017
Accepted for publication 30 January 2018
Published 15 March 2018 Volume 2018:11 Pages 1423—1432
DOI https://doi.org/10.2147/OTT.S148496
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Dr William Cho
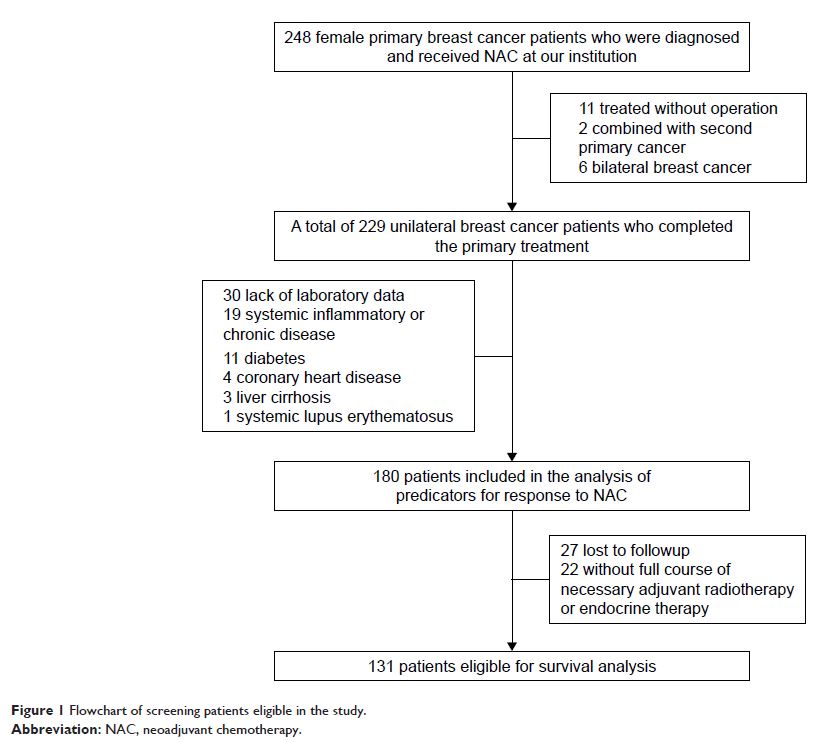
Introduction: Neoadjuvant chemotherapy (NAC) has become a standard treatment for
locally advanced breast cancer. The present study was designed to investigate
the predictive value of different peripheral inflammation/immune biomarker
responses to NAC and prognosis in breast cancer patients.
Materials and
methods: A total of 180 breast cancer
patients treated with NAC in the First Affiliated Hospital with Nanjing Medical
University between January 2008 and March 2015 were enrolled in the study. The
associations between inflammation/immune indicators and pathological complete
response (pCR) were determined, and the prognostic value of inflammation/immune
indicators was also evaluated.
Results: In the univariate analysis, patients with a high pretreatment peripheral
lymphocyte count (>2.06×109/L) showed a higher pCR rate than those with a low lymphocyte count
(23.9% vs 10.4%, P =0.023). The pCR
rate of patients with a neutrophil: lymphocyte ratio ≤2.15 was significantly
higher than that of patients with a high neutrophil: lymphocyte ratio (20% vs
7.8%; P =0.03). However, multivariate
analysis revealed that only the high lymphocyte count was predictive for pCR
(odds ratio: 4.375, 95% CI: 1.429–13.392, P =0.010).
In the survival analysis, patients with a higher neutrophil count (>2.65×109/L) were confirmed to have a shorter disease-free survival (hazard
ratio: 4.322, 95% CI: 1.028–18.174, P =0.046), and the
high neutrophil count was significantly associated with lymphovascular invasion
(P =0.037).
Conclusion: We demonstrated that a high level of baseline peripheral lymphocyte count
can be a predictor for high efficacy of NAC for breast cancer patients, and low
baseline peripheral neutrophil count may contribute to the favorable
disease-free survival.
Keywords: breast cancer, lymphocytes, neoadjuvant chemotherapy, neutrophils, pathologic
complete response