108985
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

糖尿病对鼻咽癌风险和生存率的影响:一项综合分析
Authors Guo G, Fu M, Wei S, Chen R
Received 21 September 2017
Accepted for publication 18 December 2017
Published 2 March 2018 Volume 2018:11 Pages 1193—1201
DOI https://doi.org/10.2147/OTT.S152217
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Amy Norman
Peer reviewer comments 2
Editor who approved publication: Dr Ingrid Espinoza
Background: Diabetes mellitus (DM) has been identified to be both a risk factor and
a prognostic factor in a variety of malignancies, but its association with the
risk and outcome of nasopharyngeal carcinoma (NPC) is still unclear. To
elucidate this issue, we systematically reviewed the evidence concerning the
association between DM status and NPC.
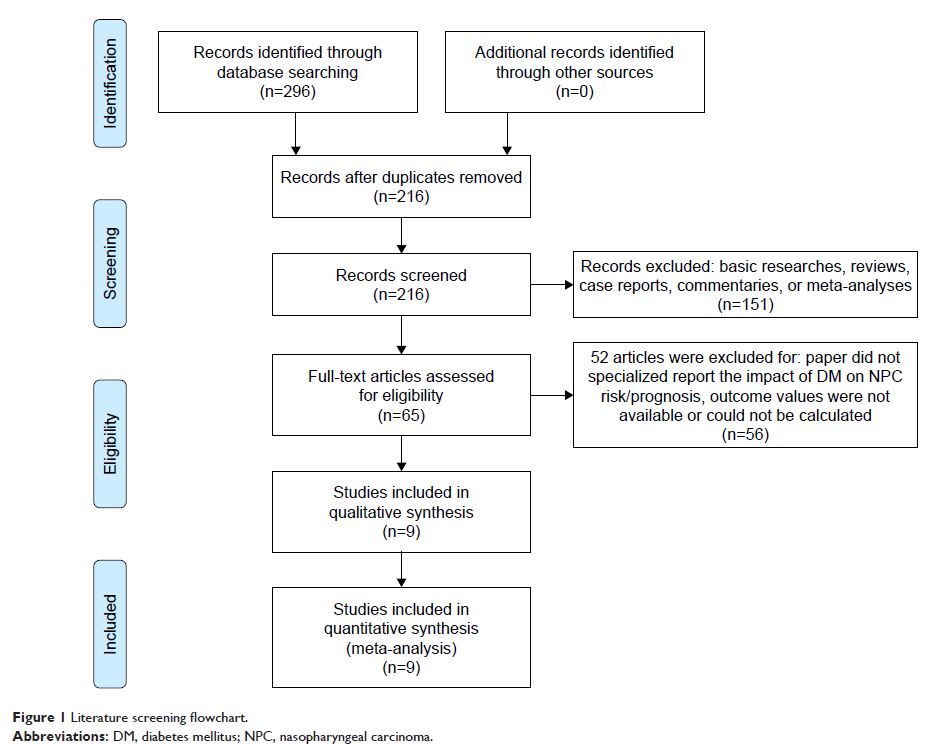
Materials and
methods: We identified studies by a
literature search of PubMed, Embase, and ISI Web of Knowledge through May 31,
2017, and by searching the reference lists of pertinent articles. Odds ratios
(ORs) and hazard ratios (HRs) with 95% CIs were used to estimate the effect
size. Heterogeneity across studies was evaluated by the Cochran’s Q and I 2 statistics.
Results: A total of nine studies were included. Four studies with a total sample
size of 221,611 reported the effect of DM on NPC risk, and the other five
studies with a sample size of 9,442 reported the impact of DM on survival in
NPC patients. All included studies were retrospective, and mostly conducted in
Asian populations. Meanwhile, condition of metformin usage was not considered
in all studies. A pooled OR of 0.65 (95% CI: 0.43–0.98, P =0.04) revealed an inverse
association between DM and NPC. Additionally, pooled analyses of studies
investigating the prognosis value of DM revealed that preexisting DM had no
effect on overall survival (HR =1.17, 95% CI: 0.94–1.46, P =0.16), local recurrence-free
survival (HR =1.16, 95% CI: 0.80–1.67, P =0.44), and
distant metastasis-free survival (HR =1.14, 95% CI: 0.92–1.40, P =0.22).
Conclusion: Our results suggested that DM patients might have decreased NPC risk,
and have little impact on prognosis of NPC patients. This conclusion should be
limited to Asian population. Our results also suggest that more attention
should be paid to metformin medication in further studies in order to clarify
whether the effects of DM on NPC risk and prognosis are influenced by the
anticancer effect of metformin.
Keywords: diabetes mellitus, nasopharyngeal carcinoma, risk factor,
prognosis factor, a meta-analysis, evidence based medicine